Dr David Hegarty
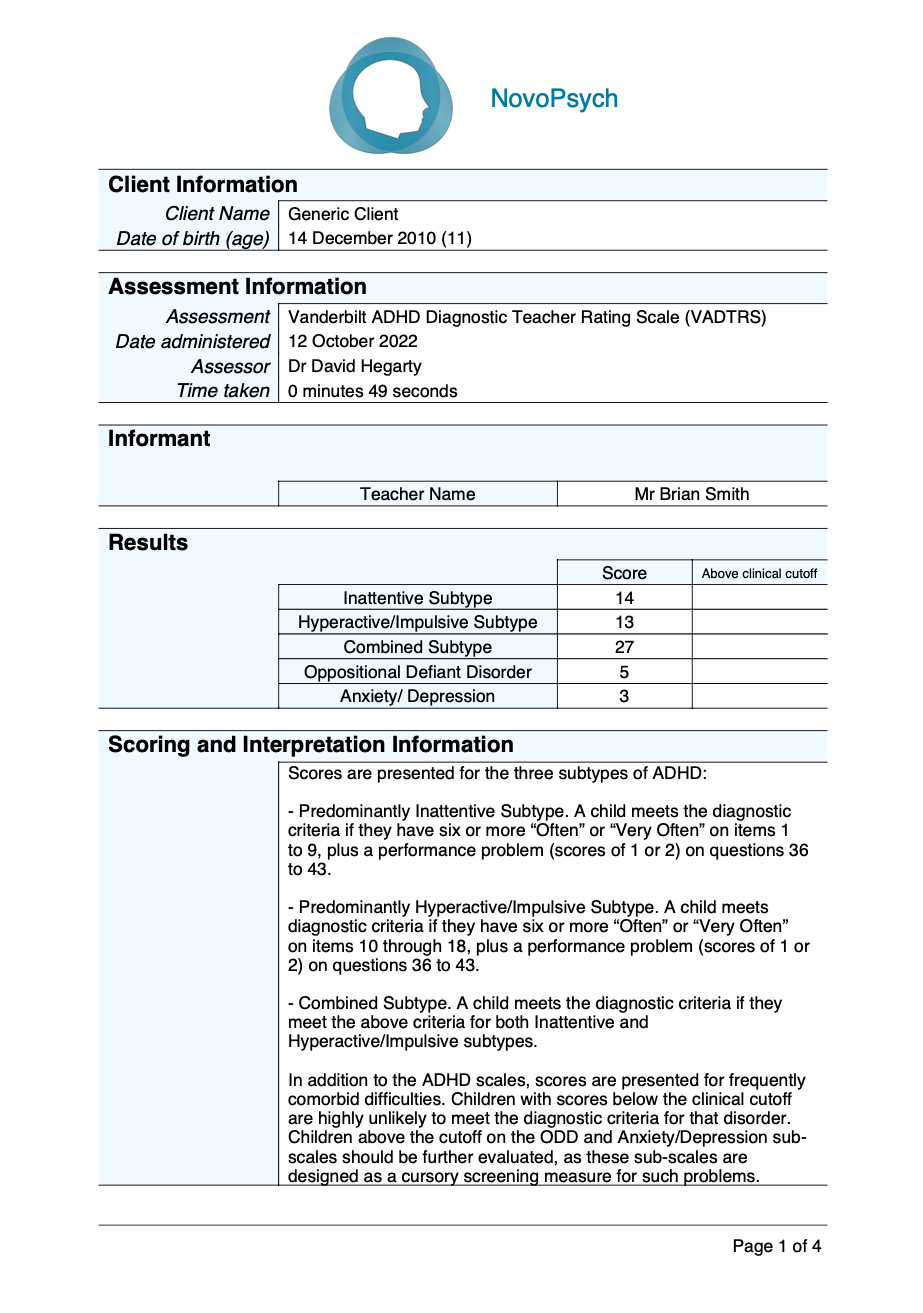
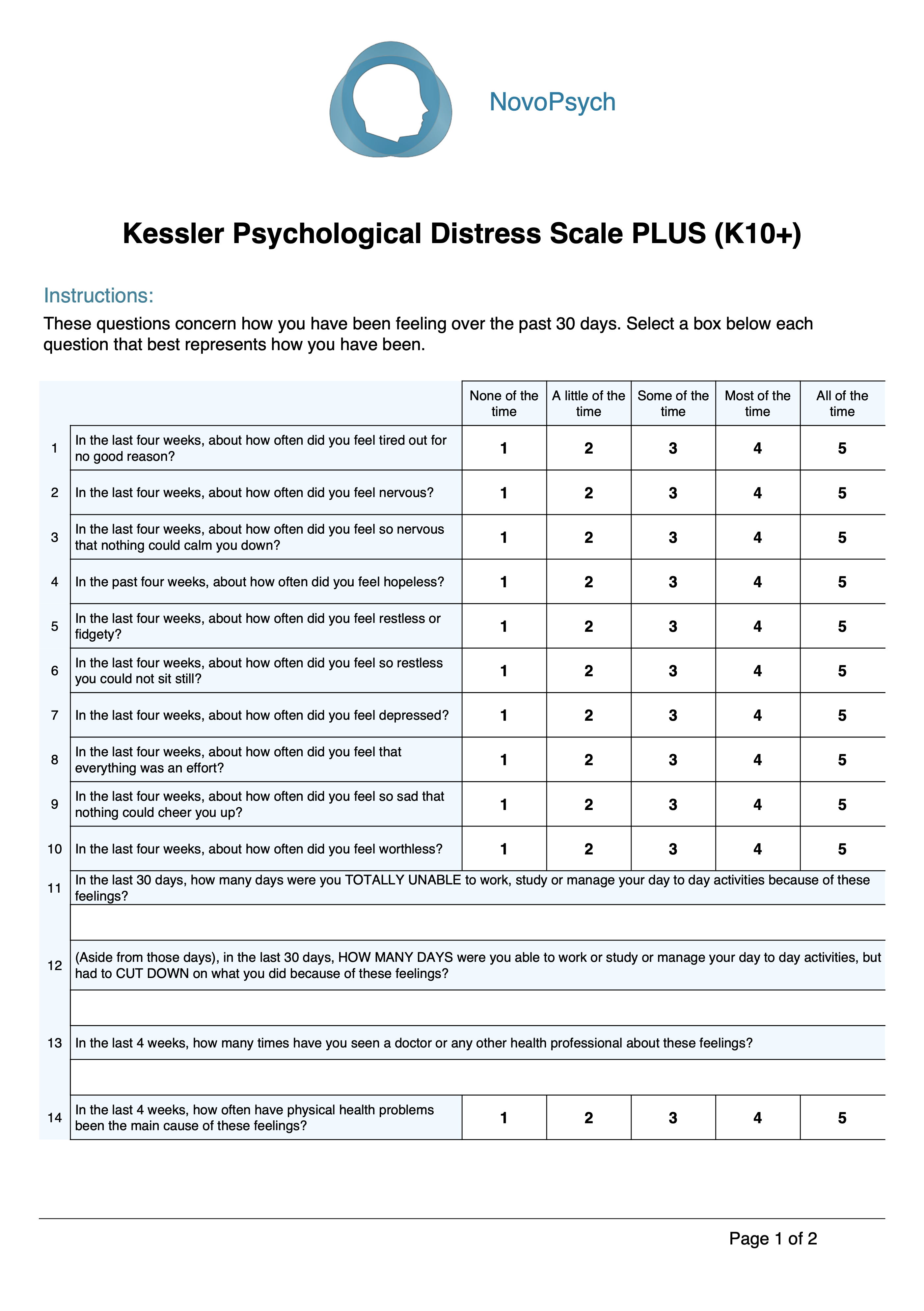
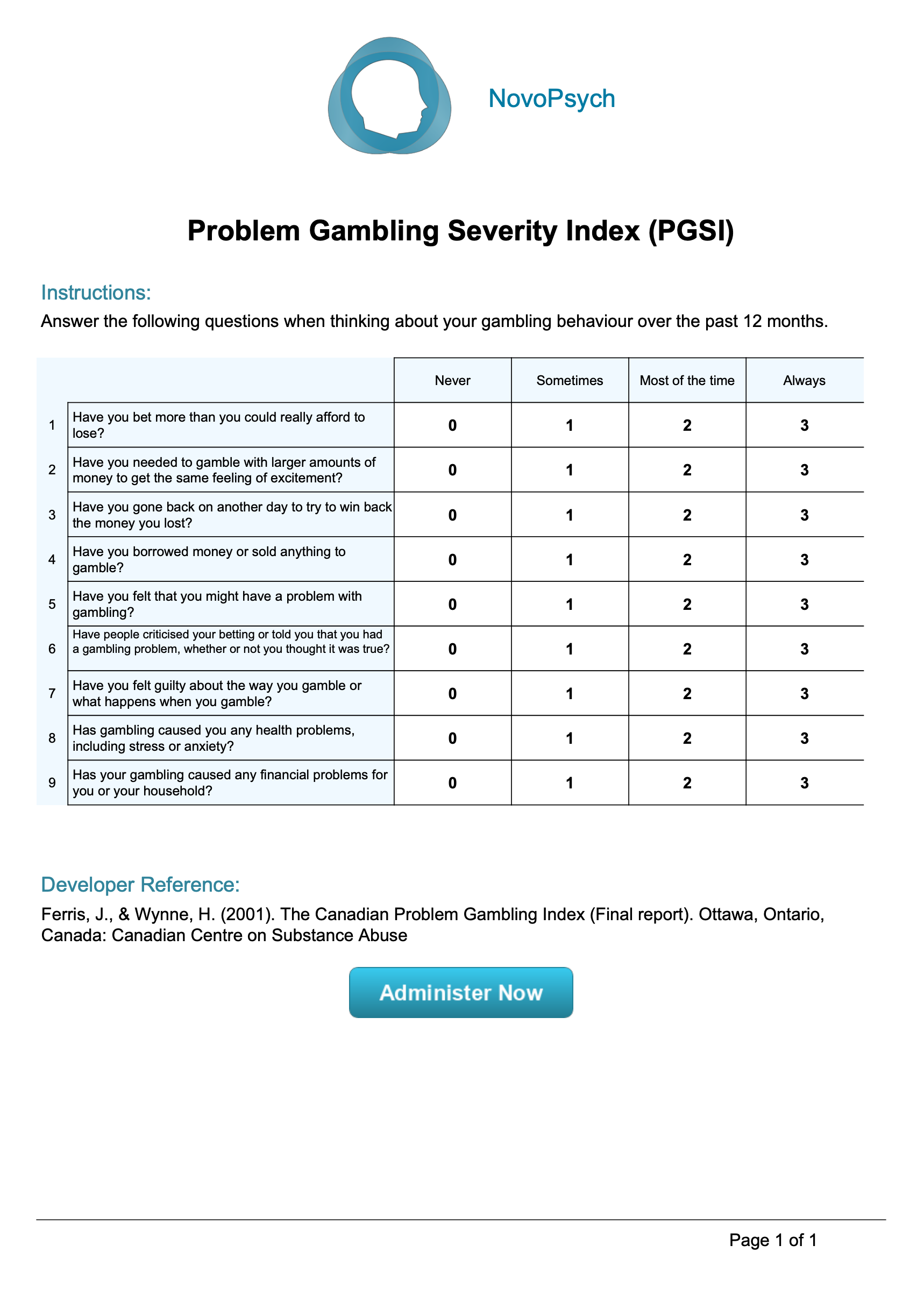
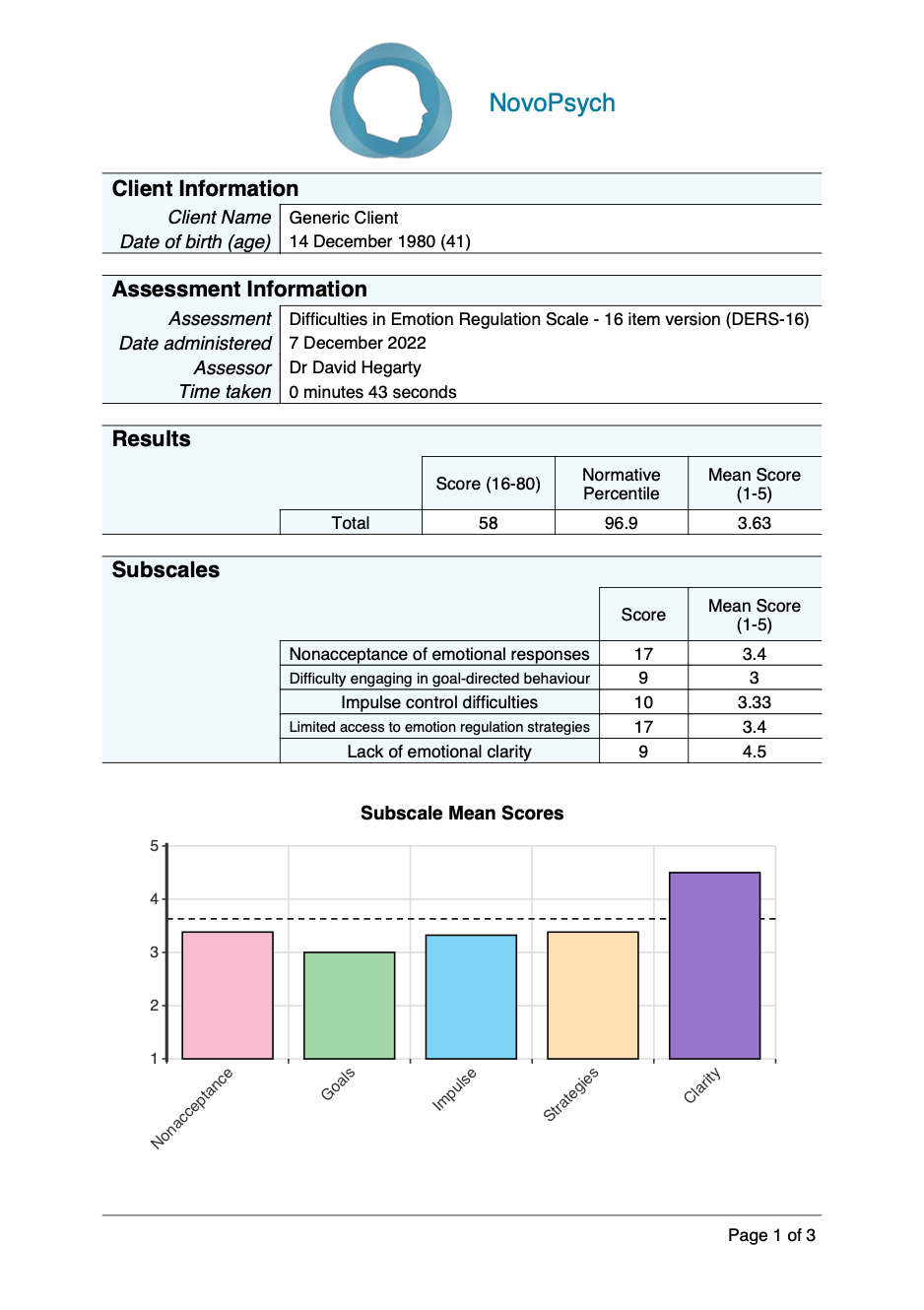
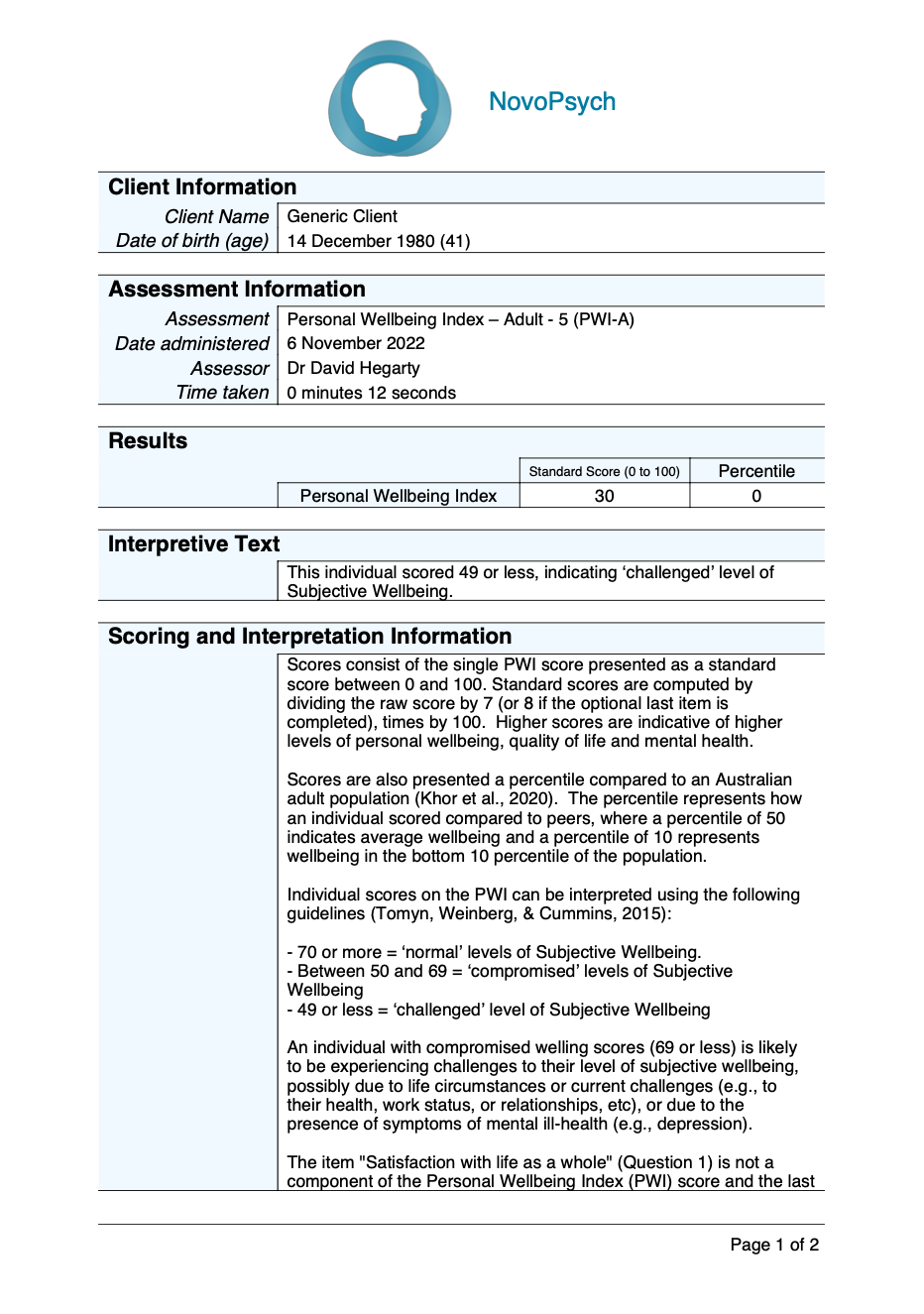
The Brief Emotional Distress Scale for Youth (BEDSY) is an 8-item self-report measure designed to assess emotional distress in young people (11-17 years). The scale assesses a general construct of emotional distress, as opposed to specific features of anxiety and depression symptoms.
- 1 minute
- Ages 11 to 17
- Adolescent, Outcome Monitoring
The BEDSY (Spence & Rapee, 2022) is suitable for use in clinical and school settings for identifying distressed clients and as a mental health screener. Given its short length, the BEDSY is suited to routine administrations during clinical treatment to monitor changes in symptoms and assess treatment progress. Additionally, its length and development for school-aged youth, makes it an ideal measure for cohort screening within a school context in order to determine students who are potentially at risk for mental health difficulties.
The BEDSY is based on a dimensional rather than a categorical conception of distress, and scores emphasise the degree to which a young person is experiencing symptoms rather than having diagnostic cutoff points.
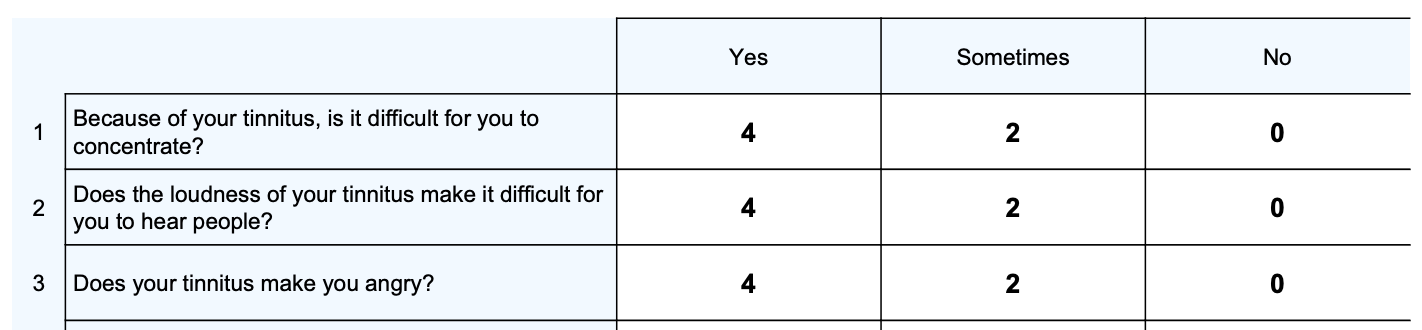
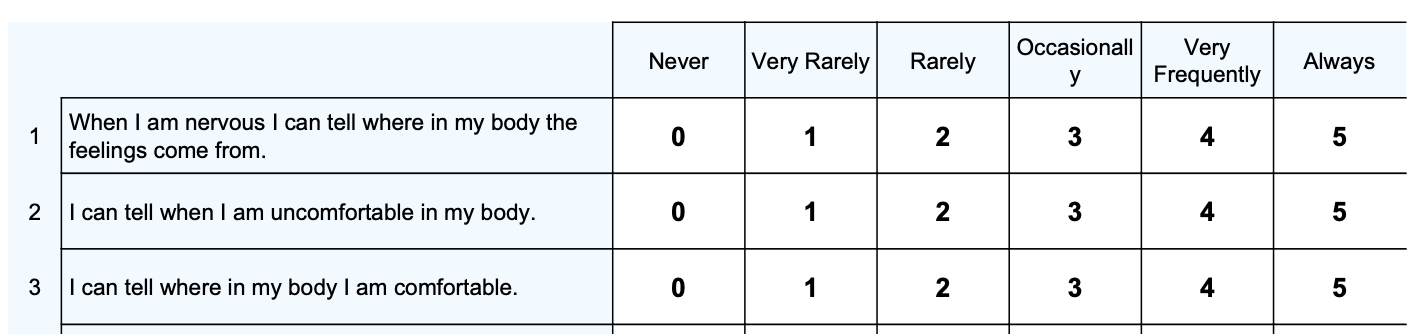
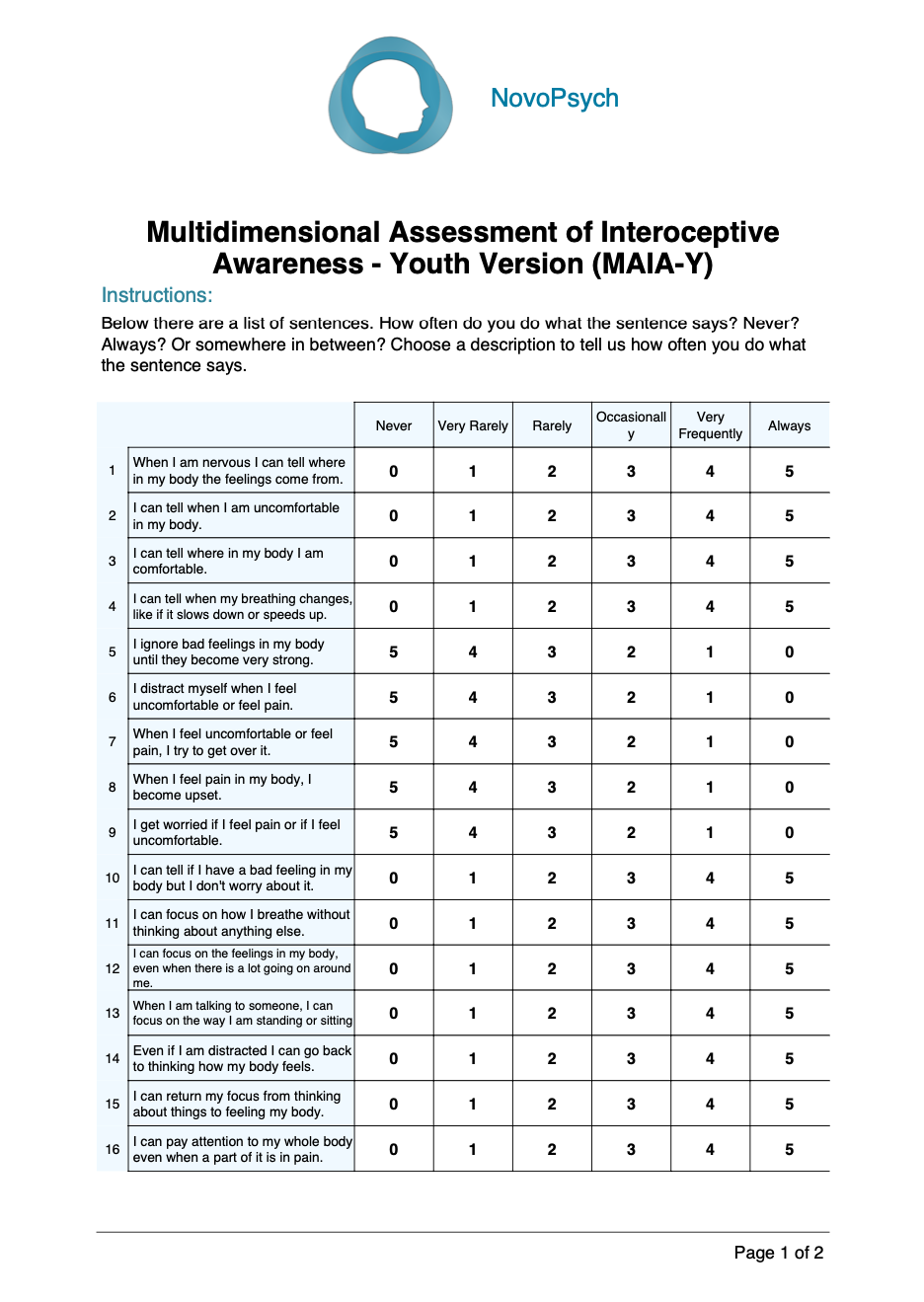
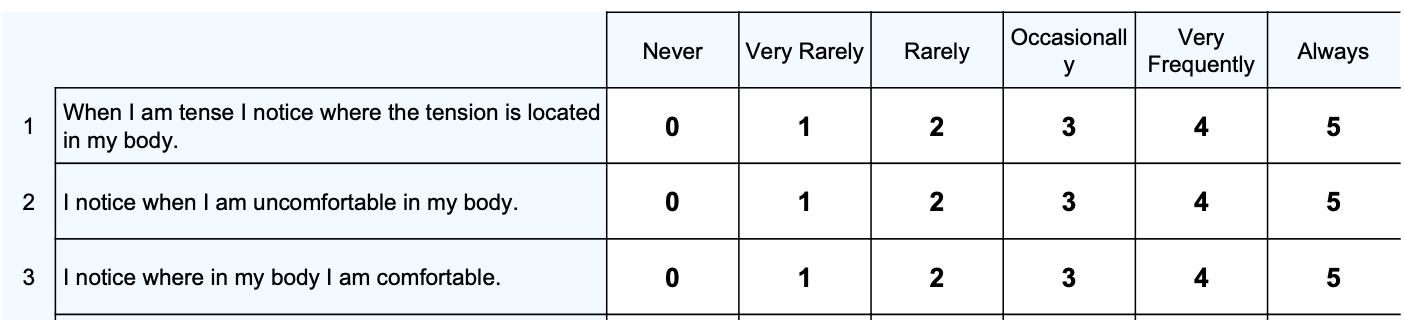
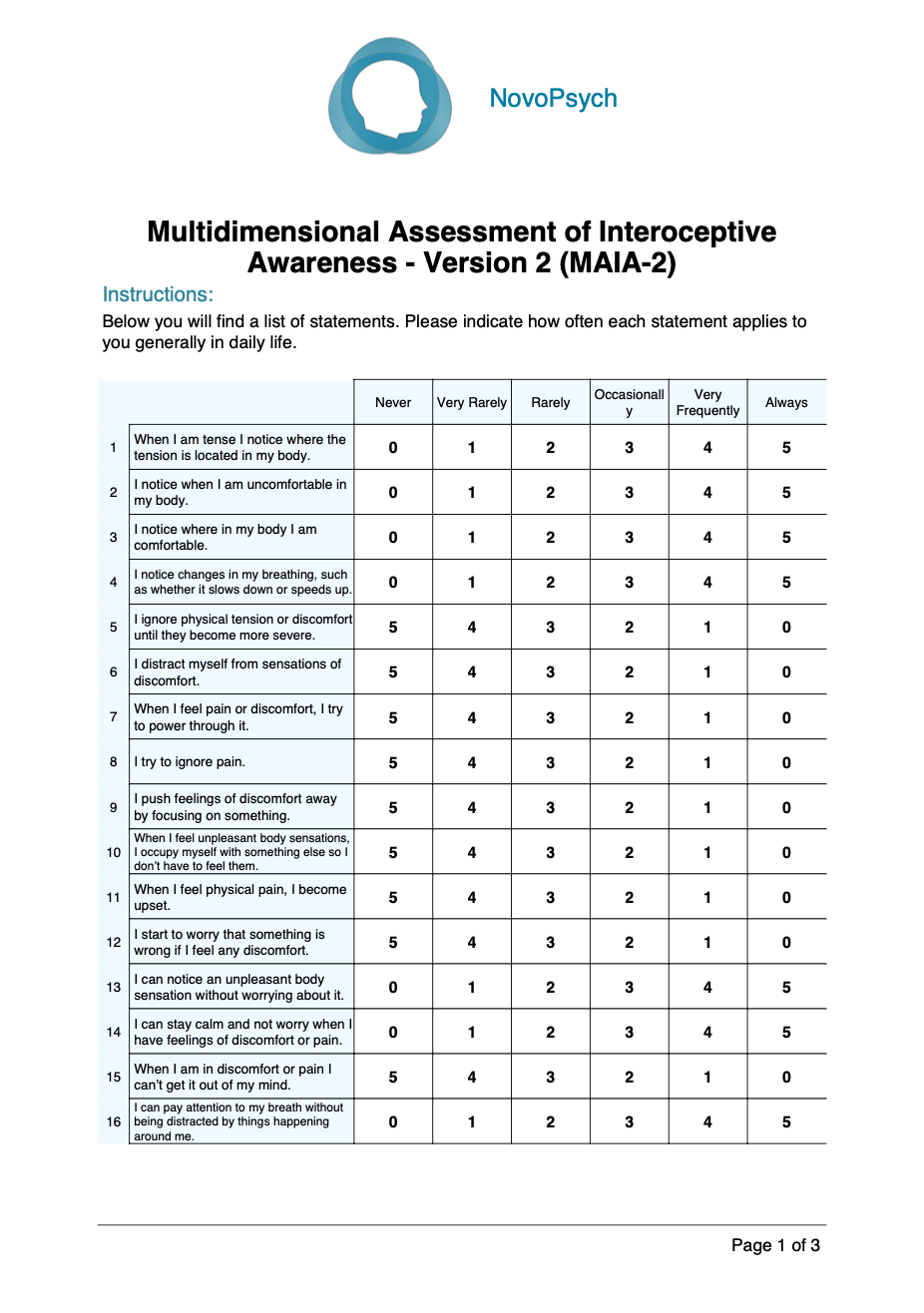
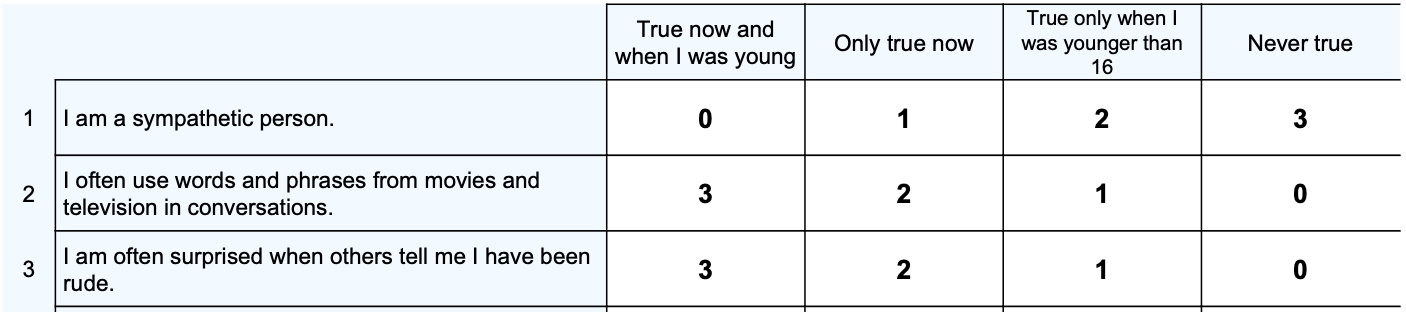
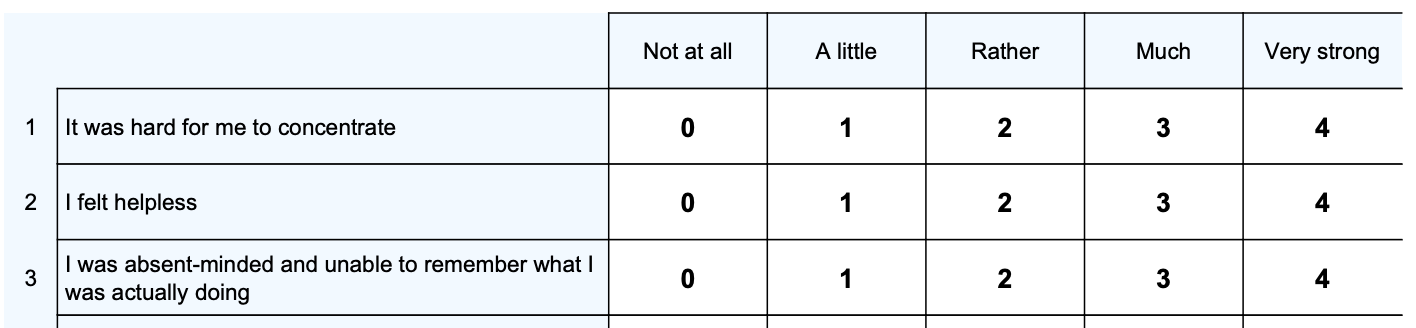
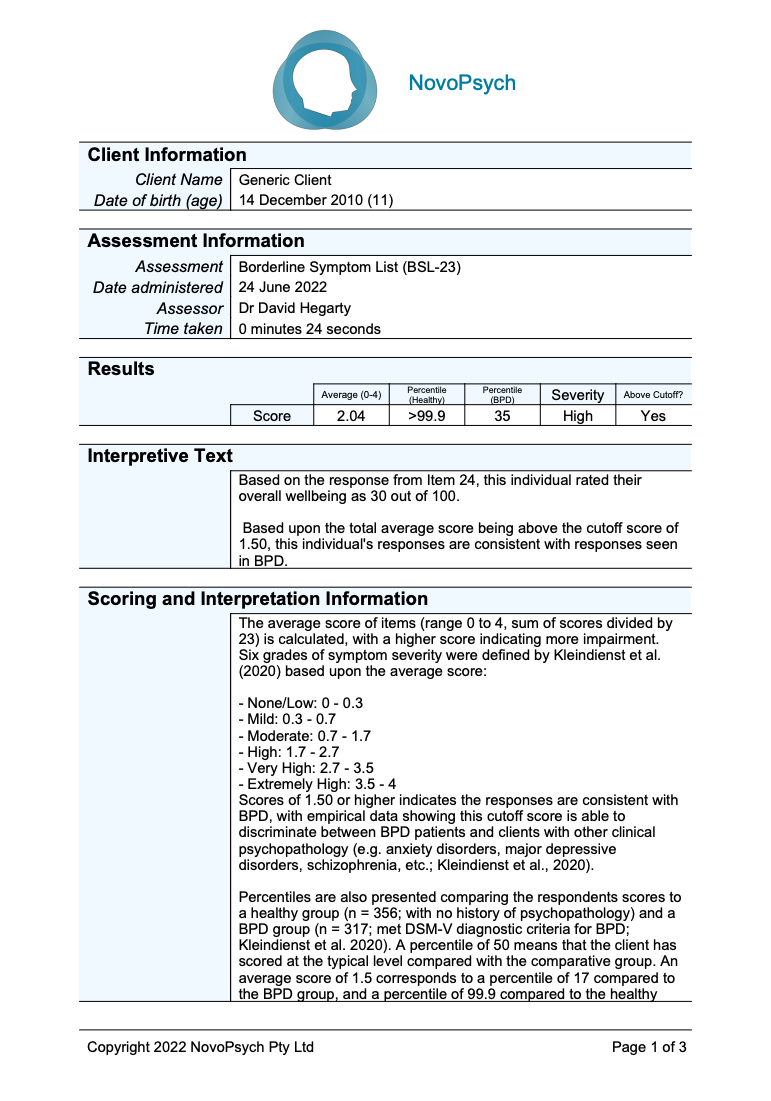
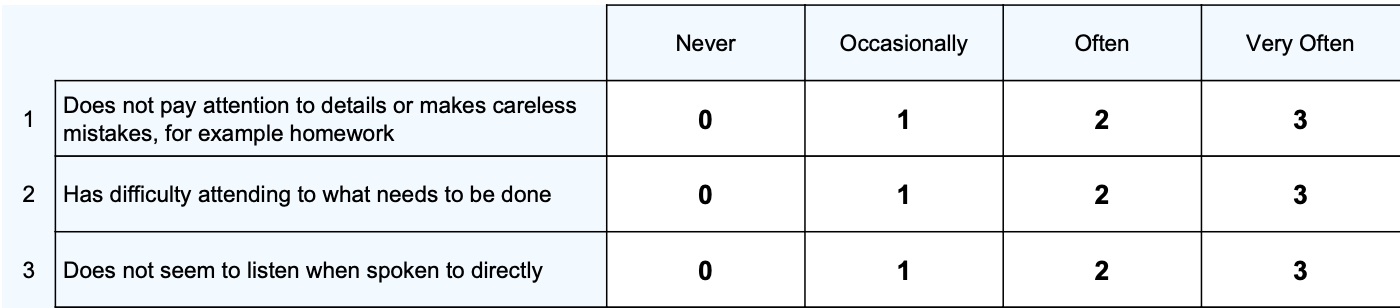
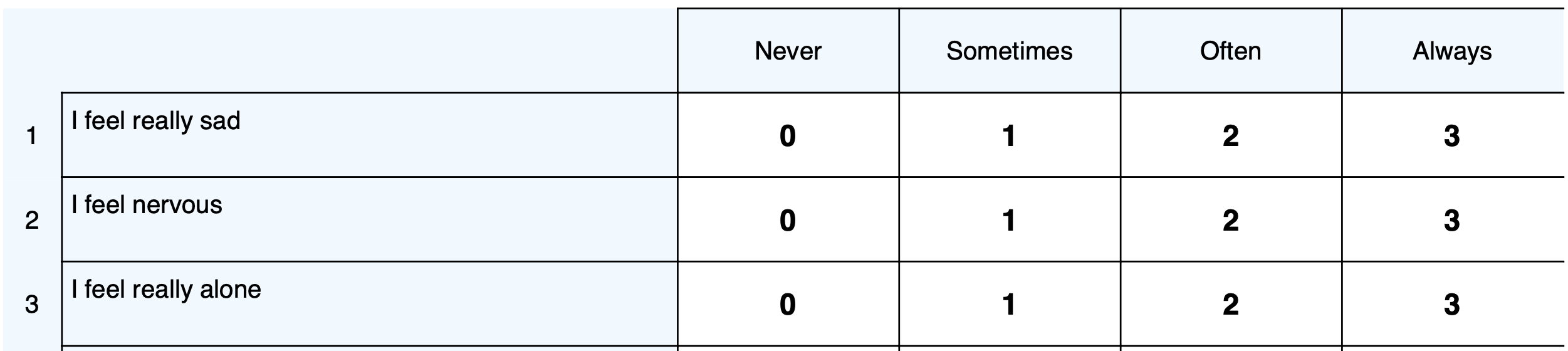
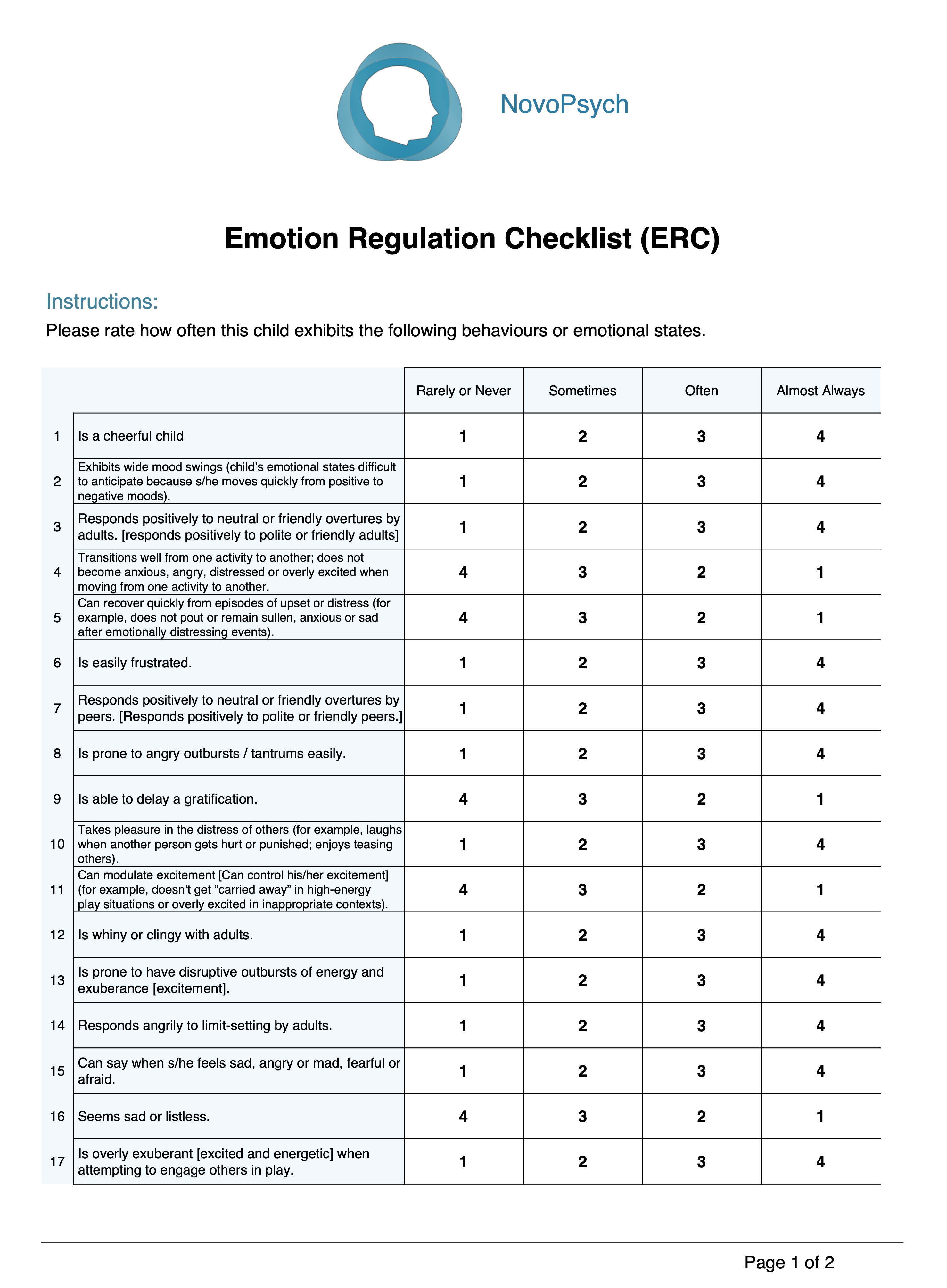
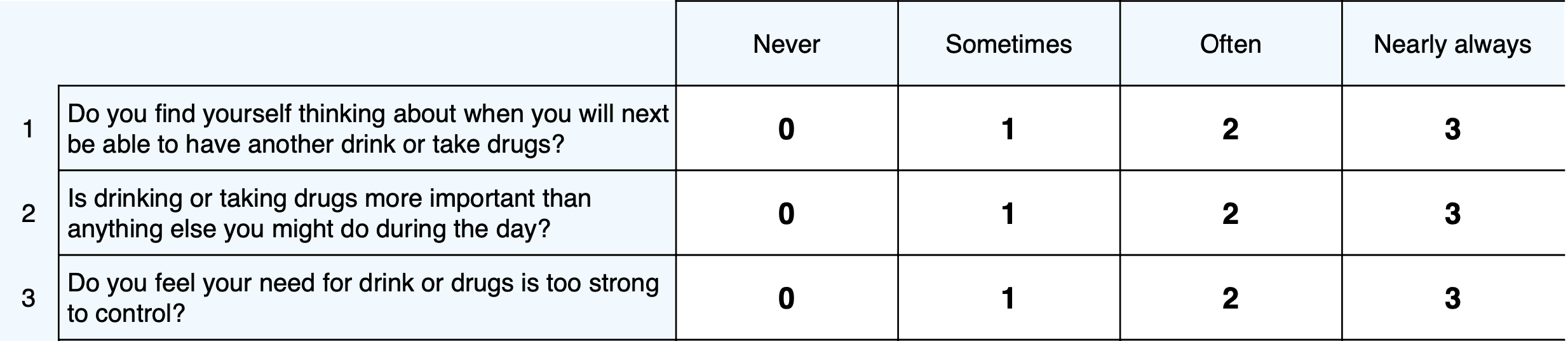
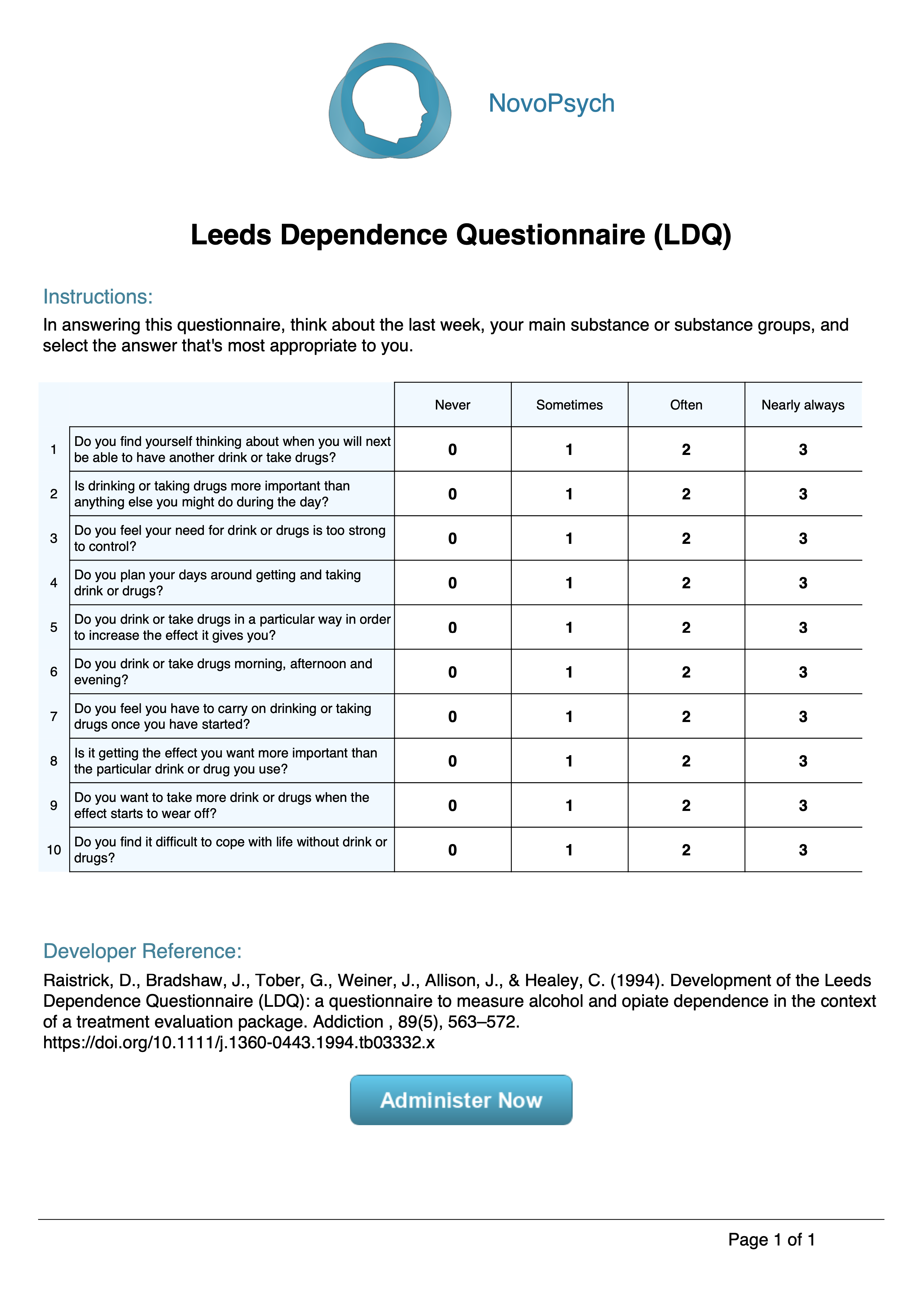
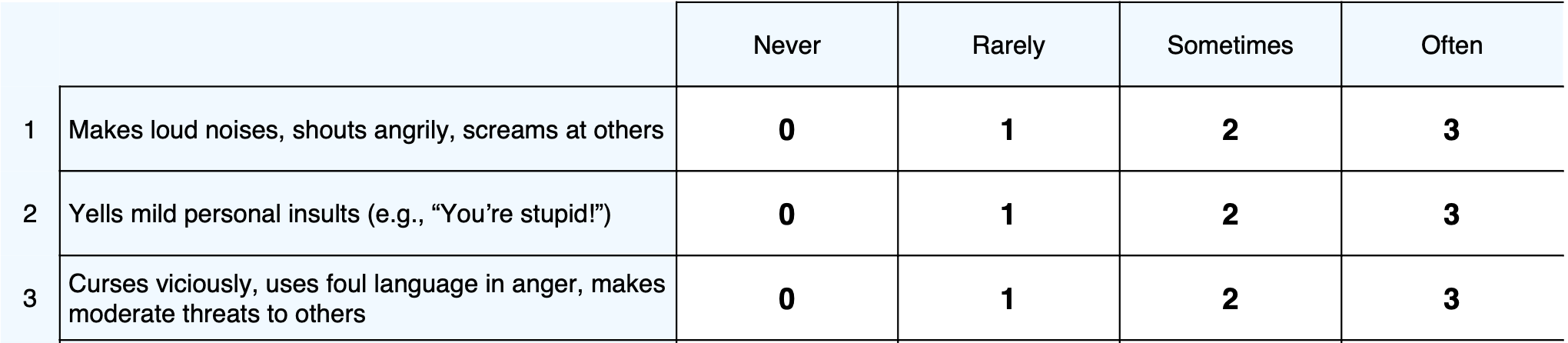
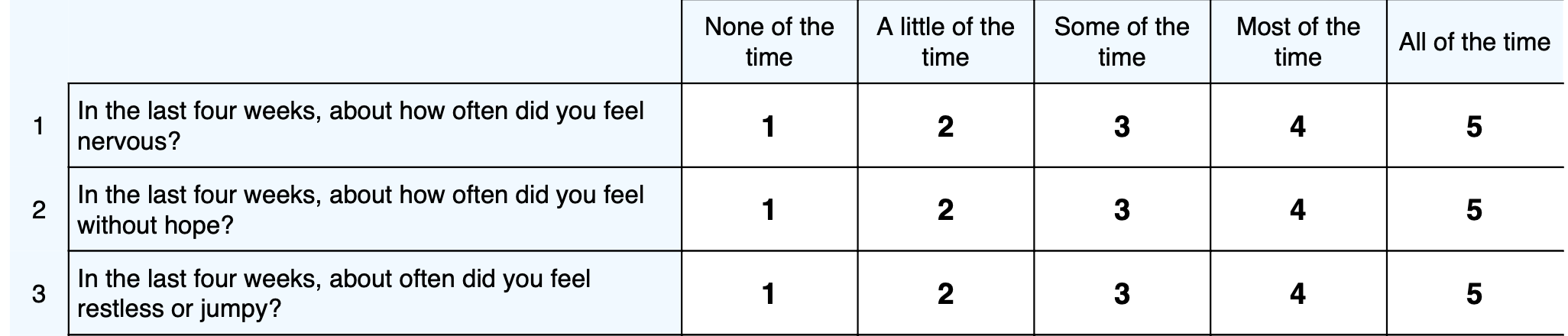
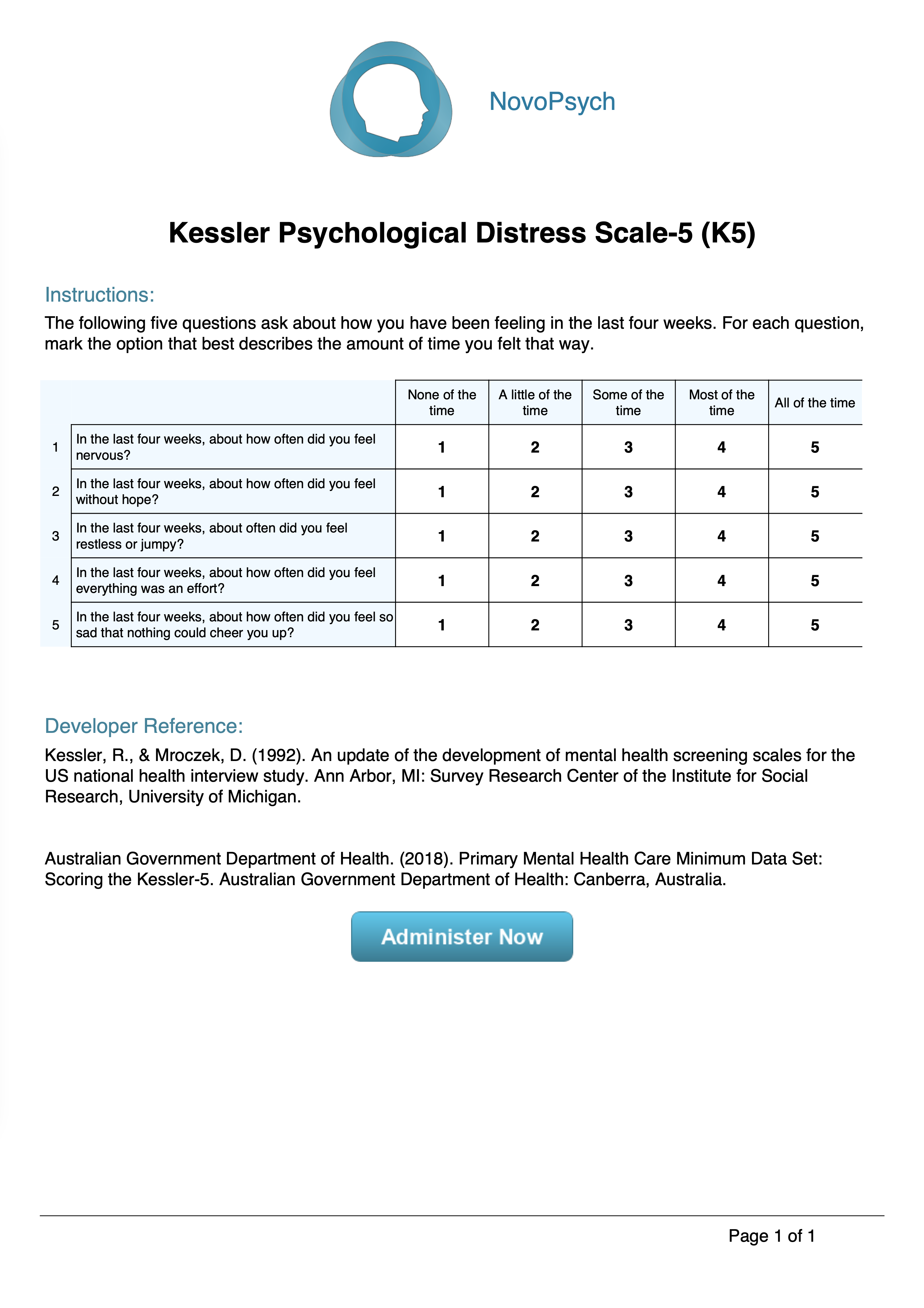
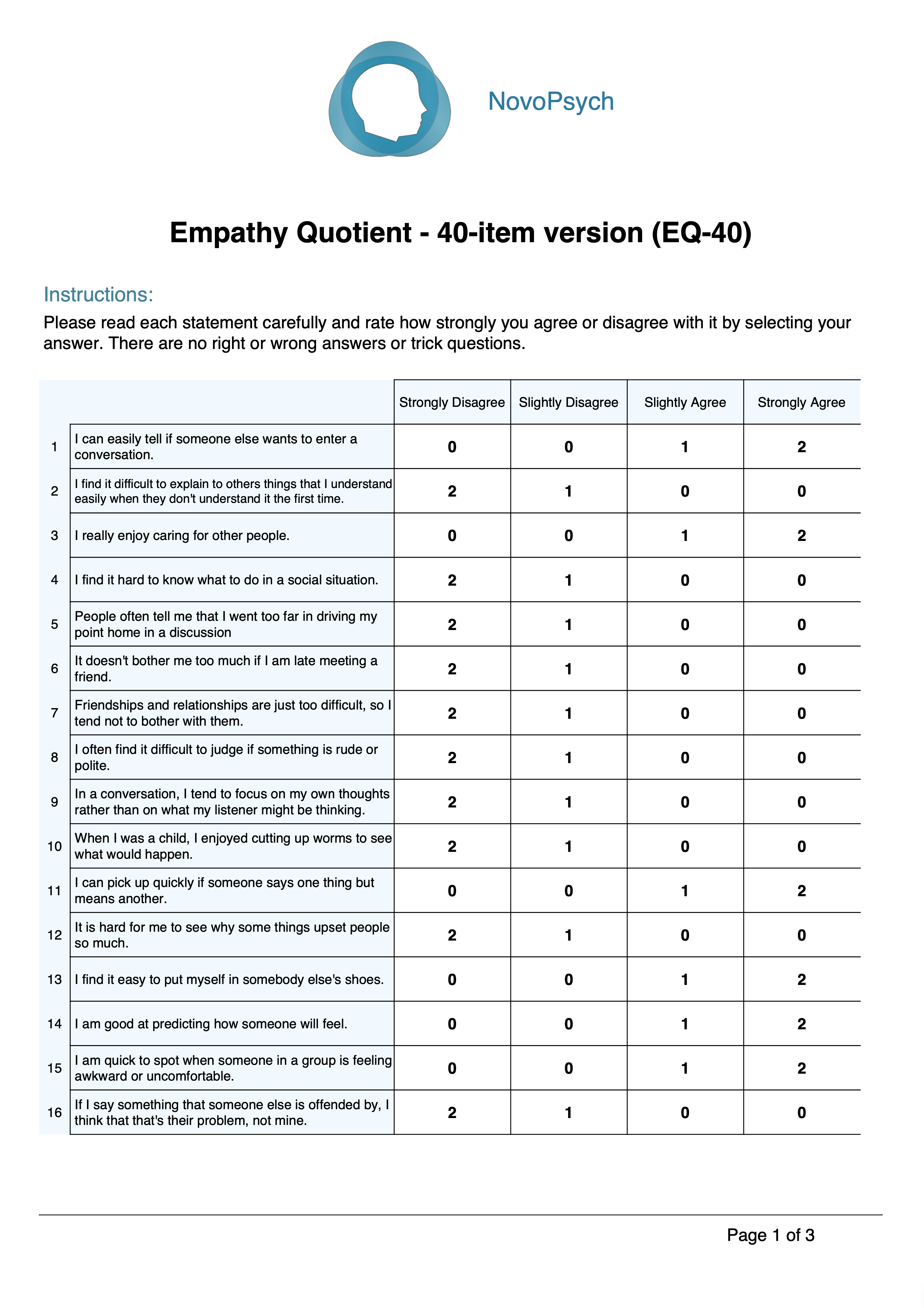
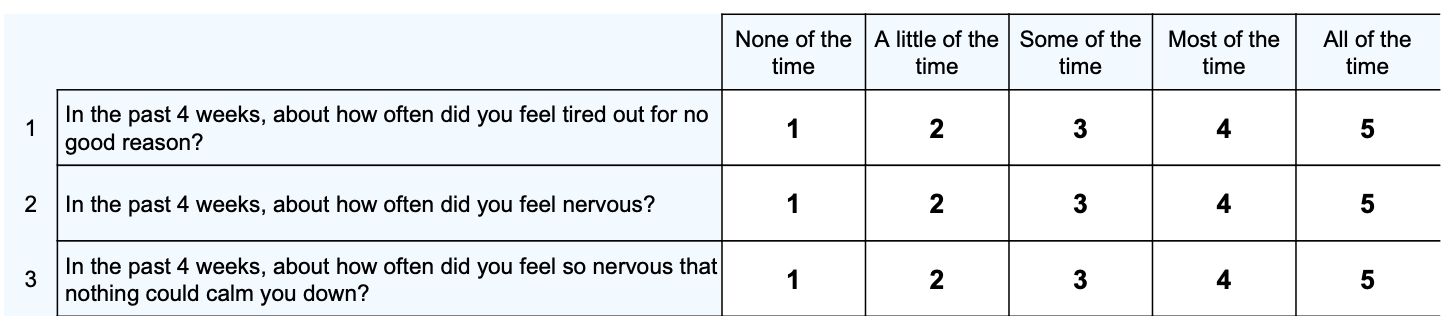
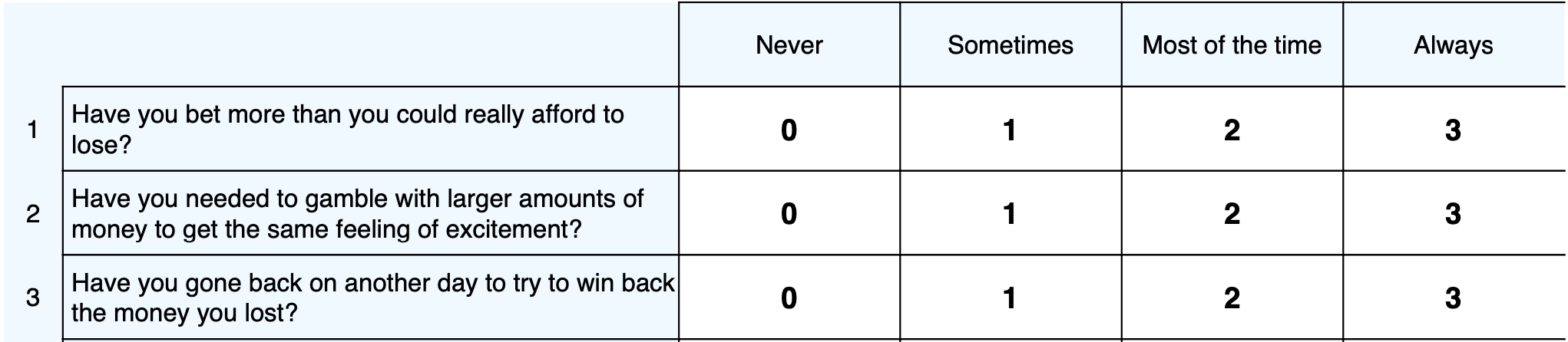
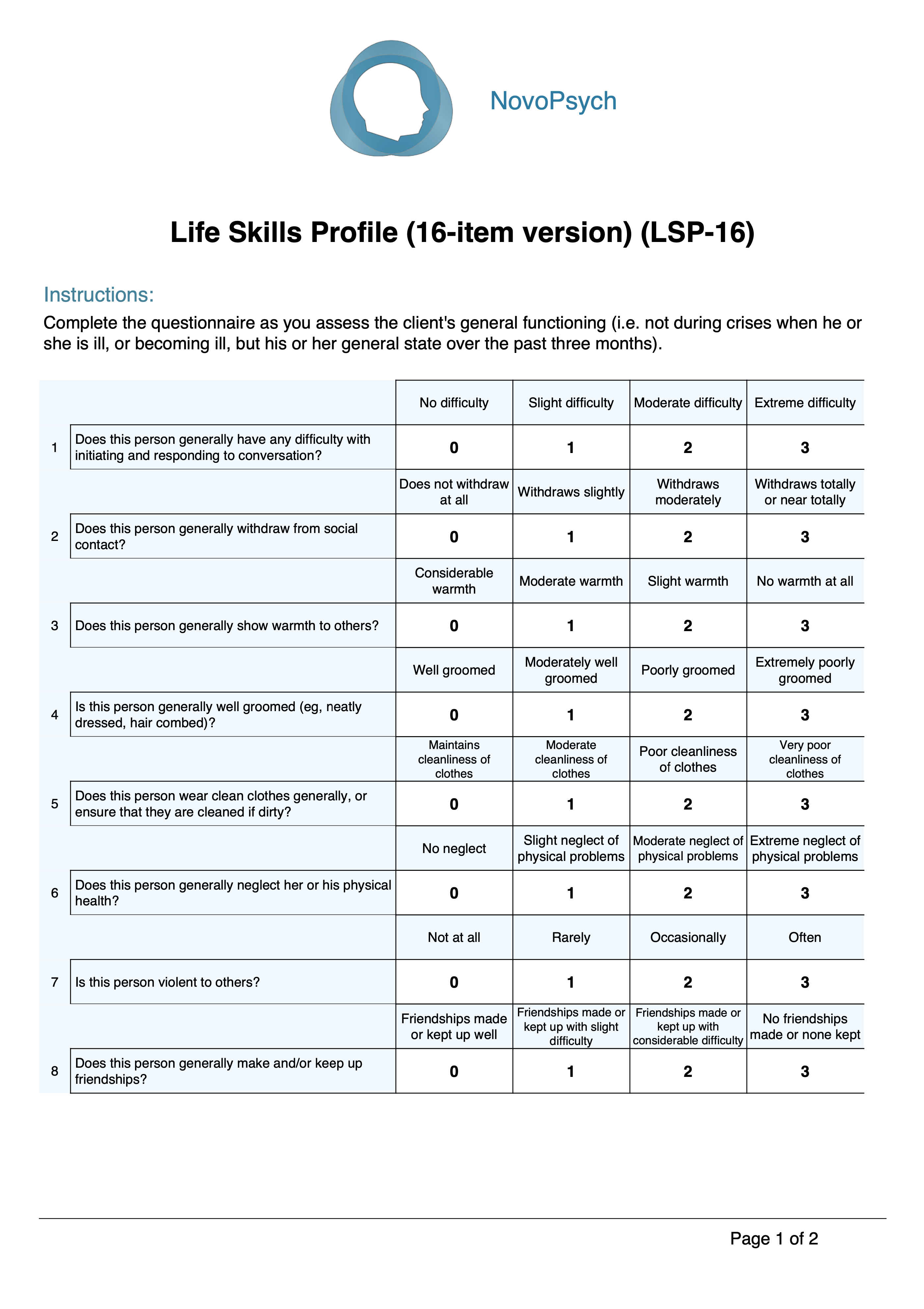
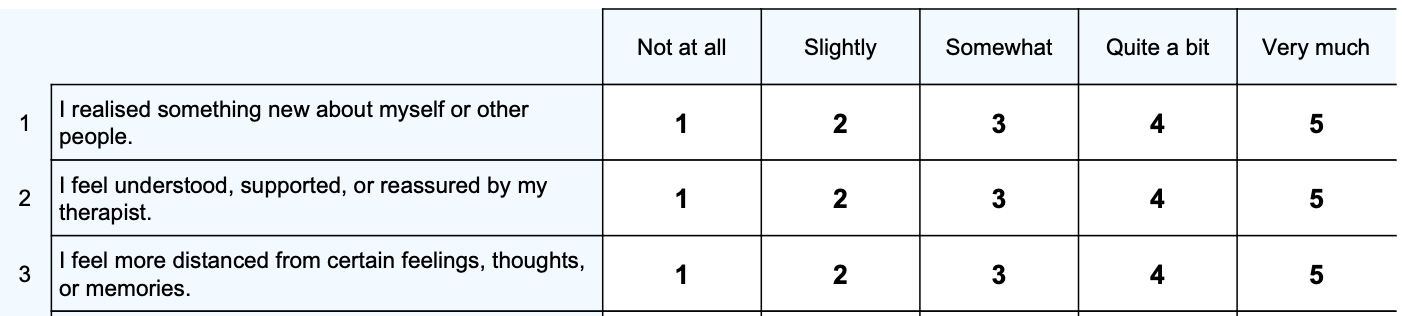
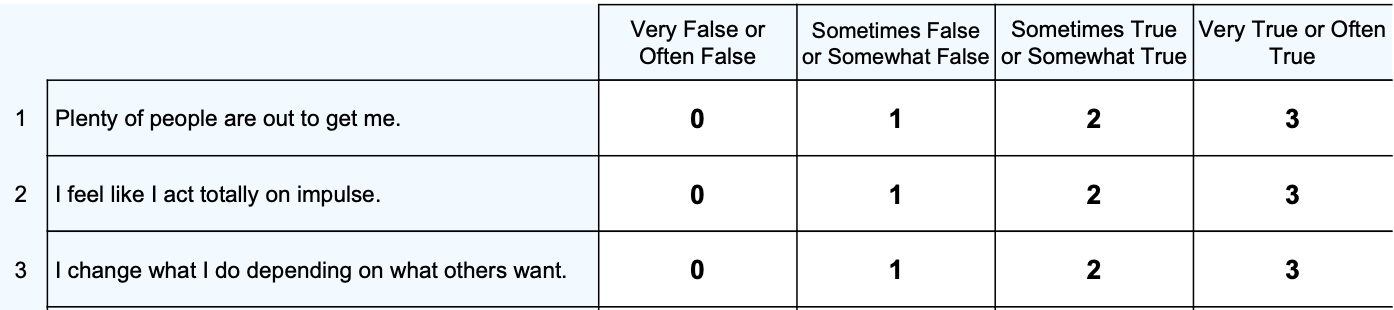
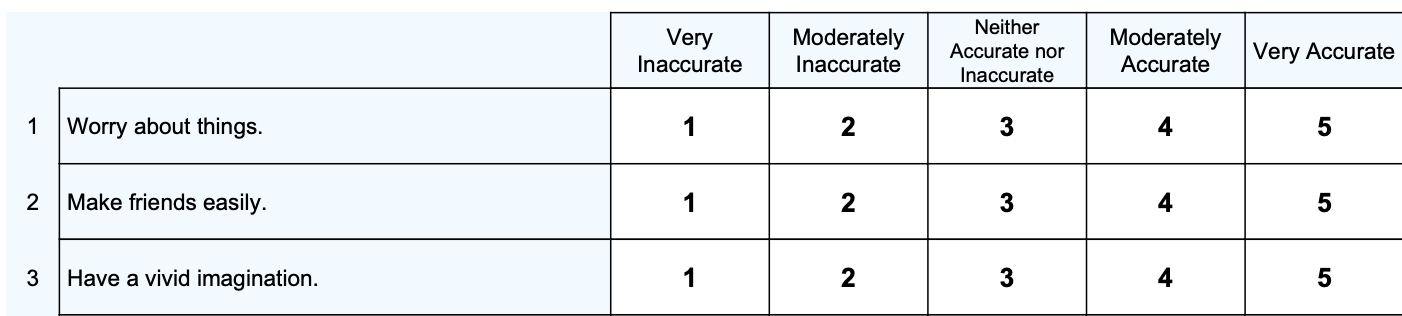
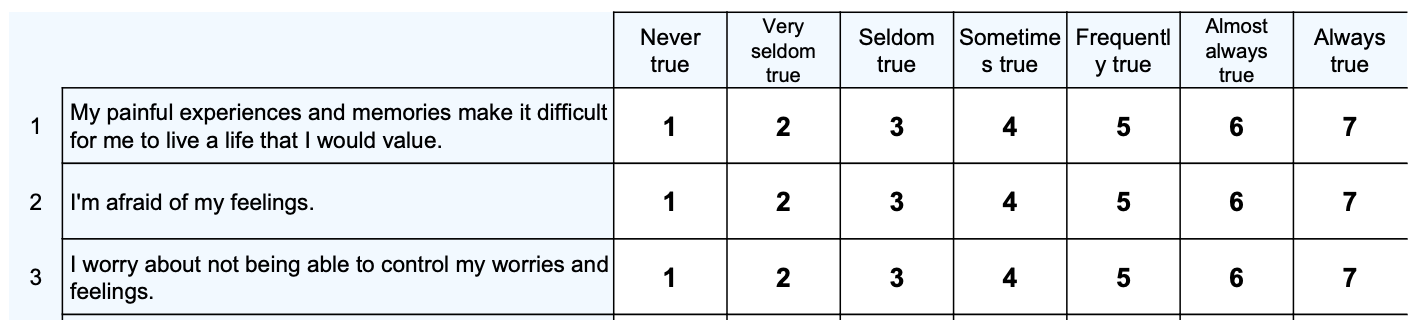
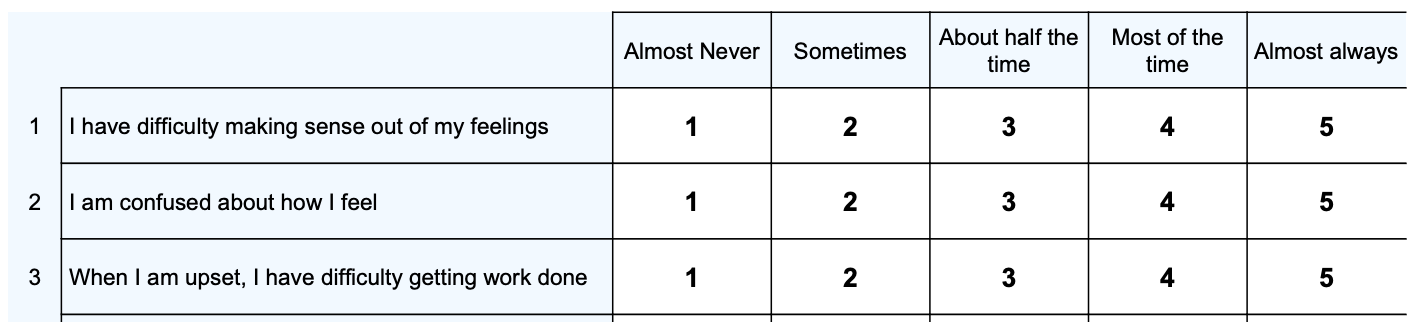
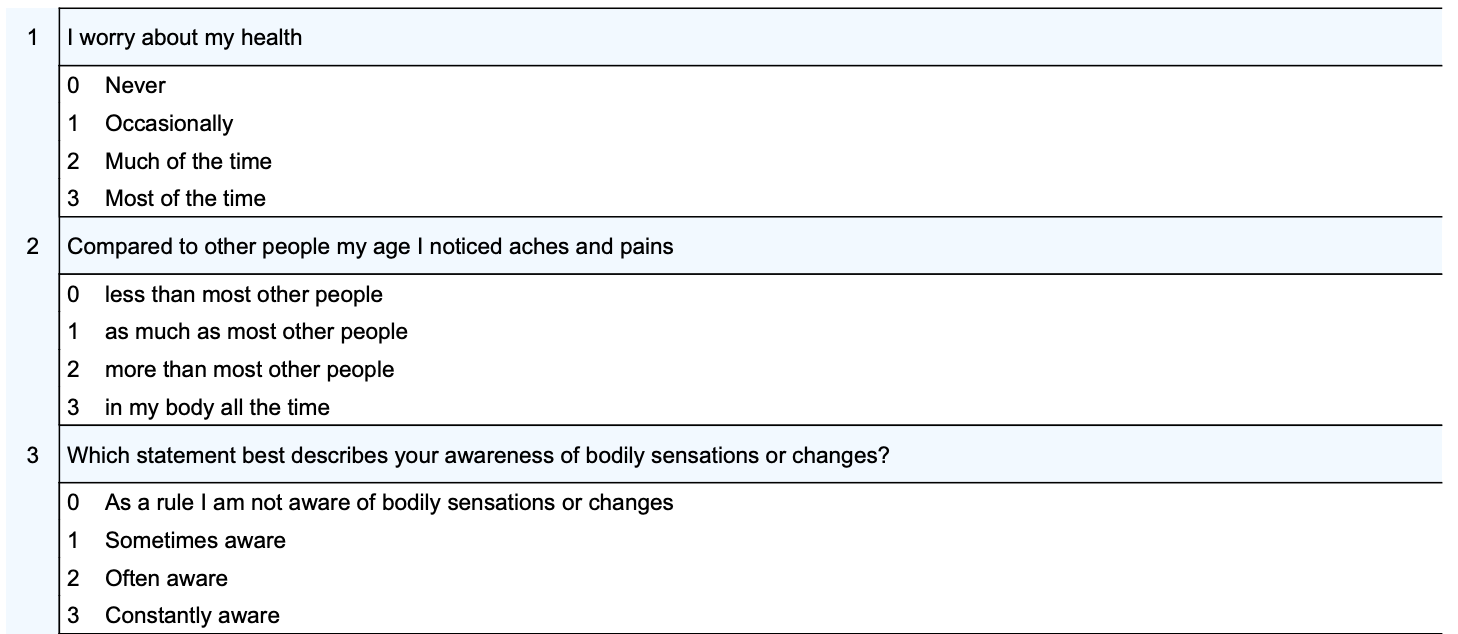
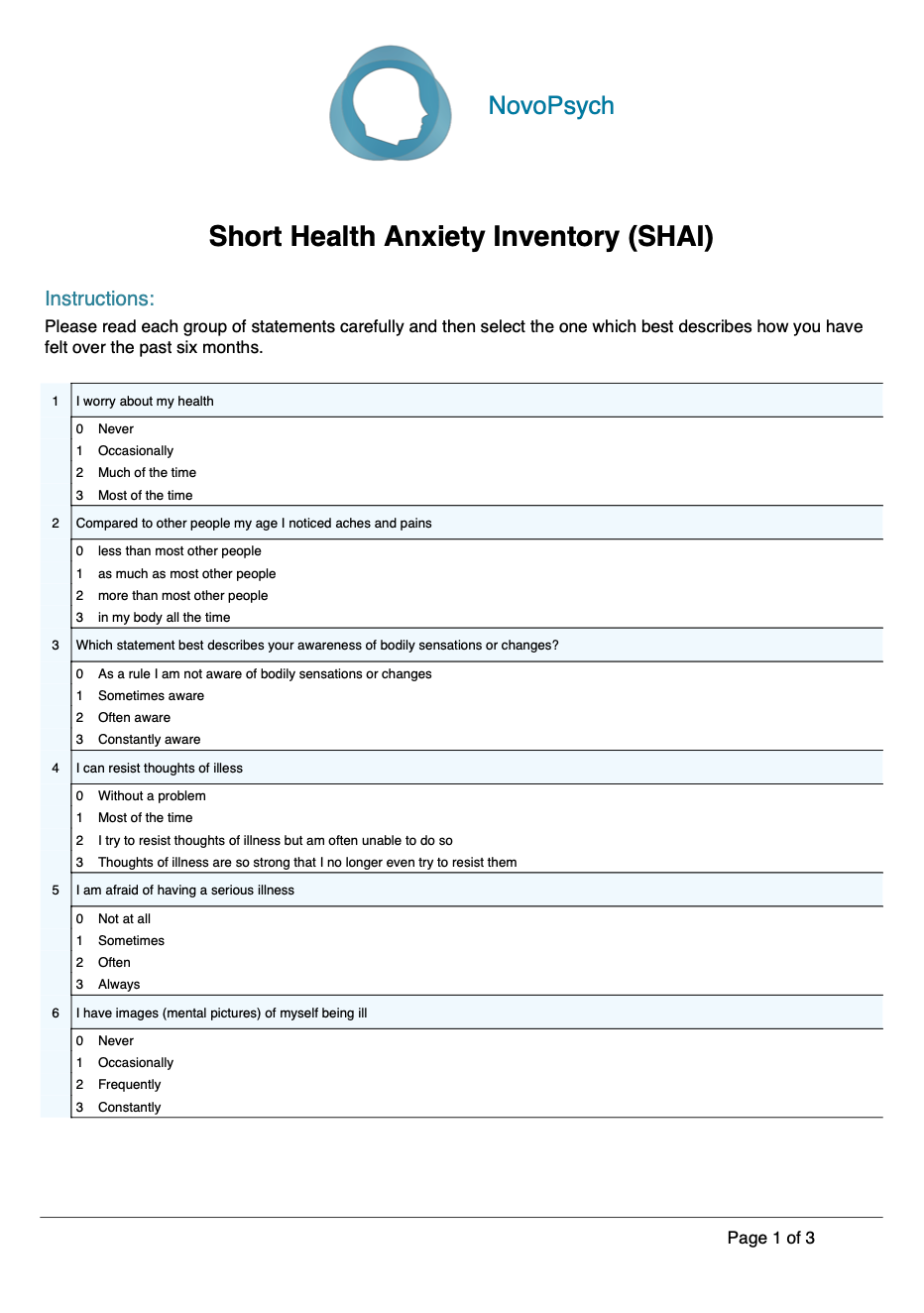
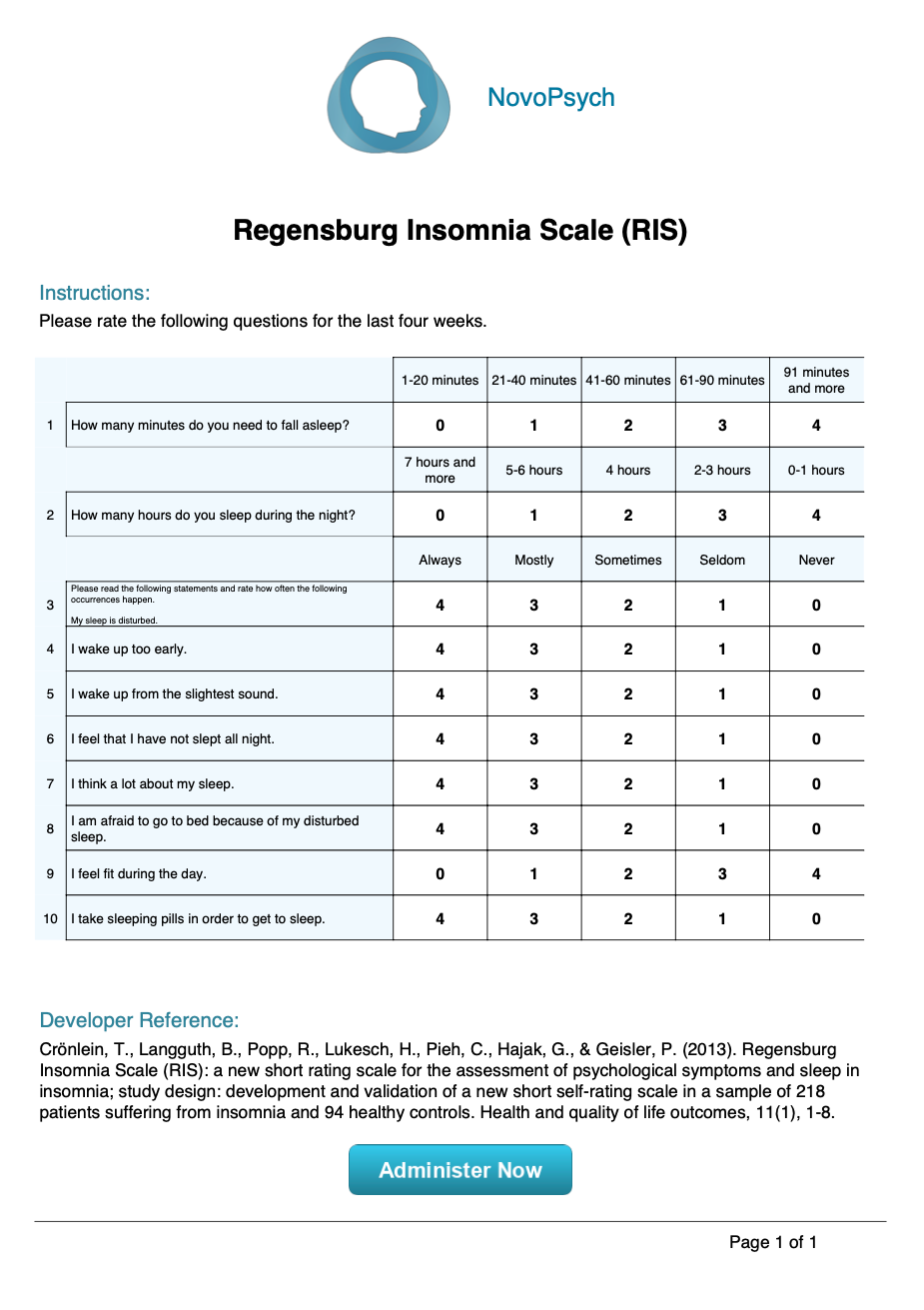
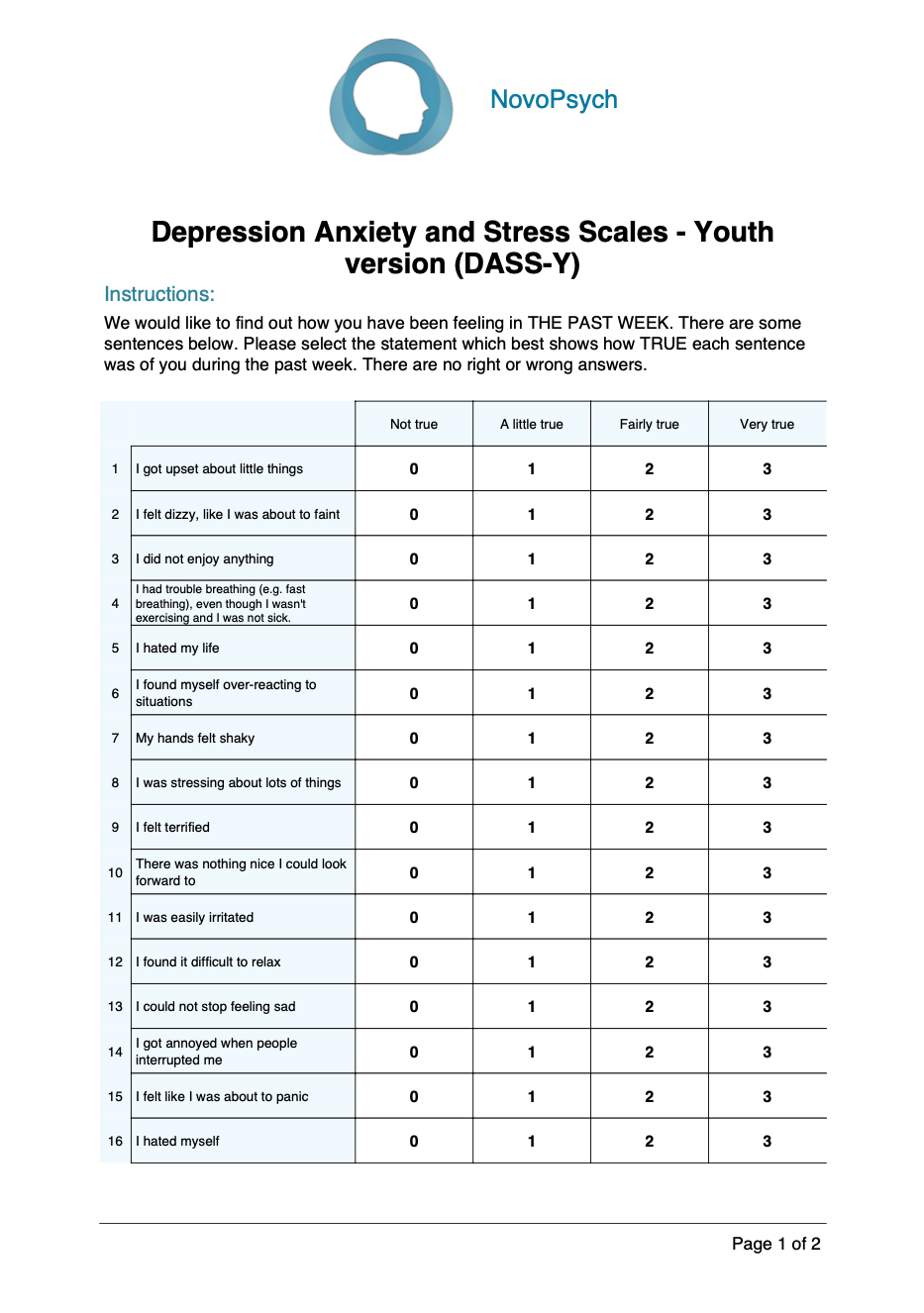
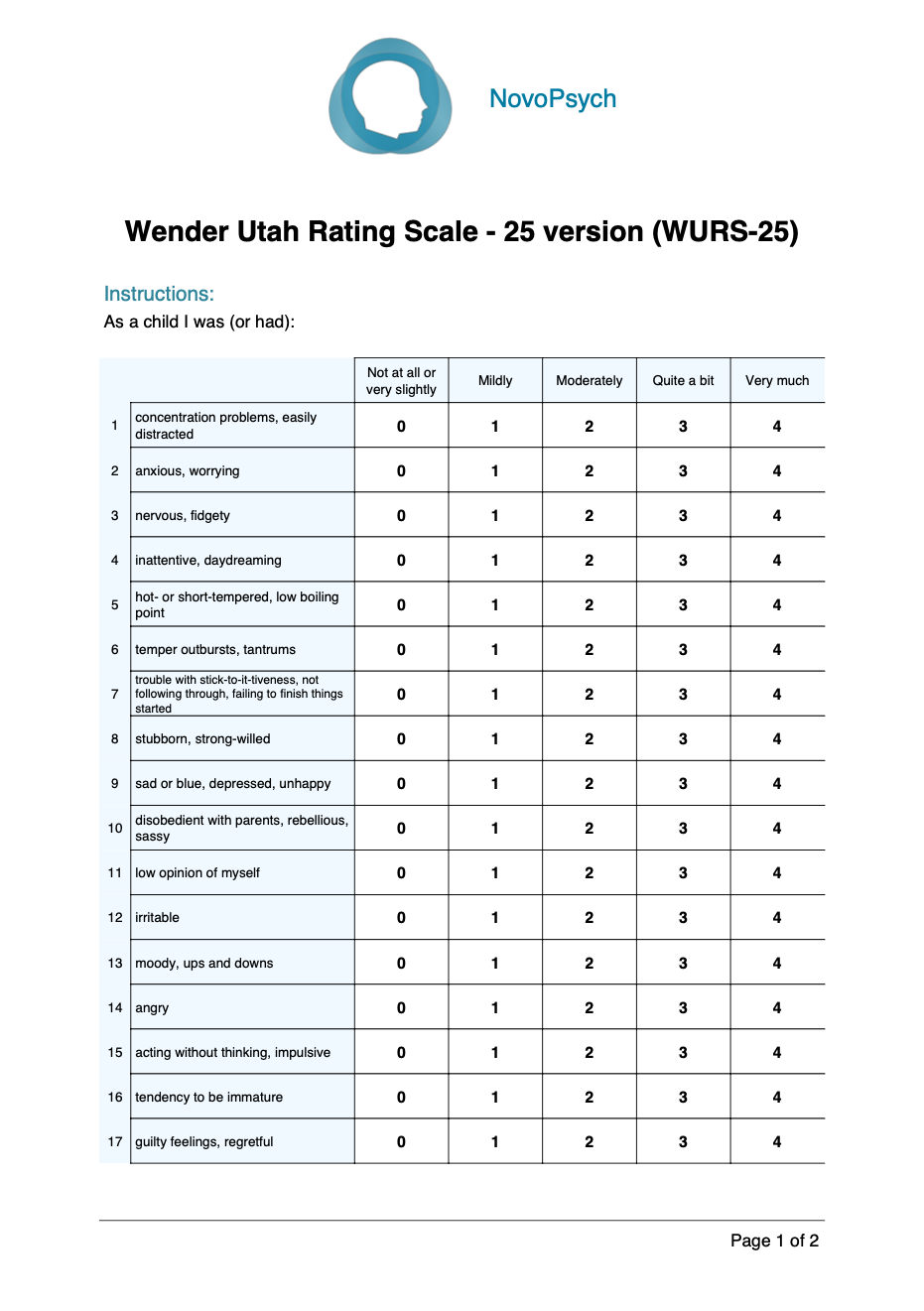
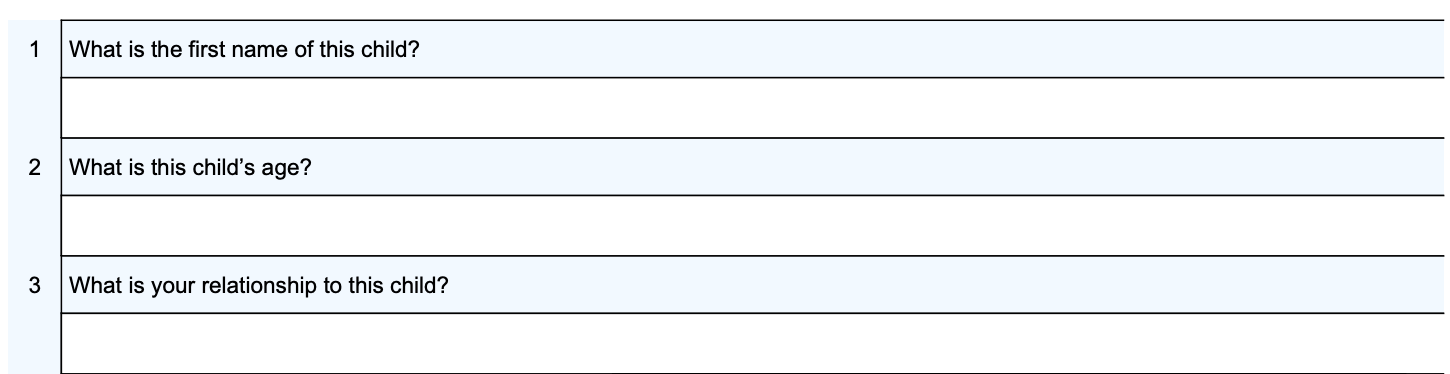
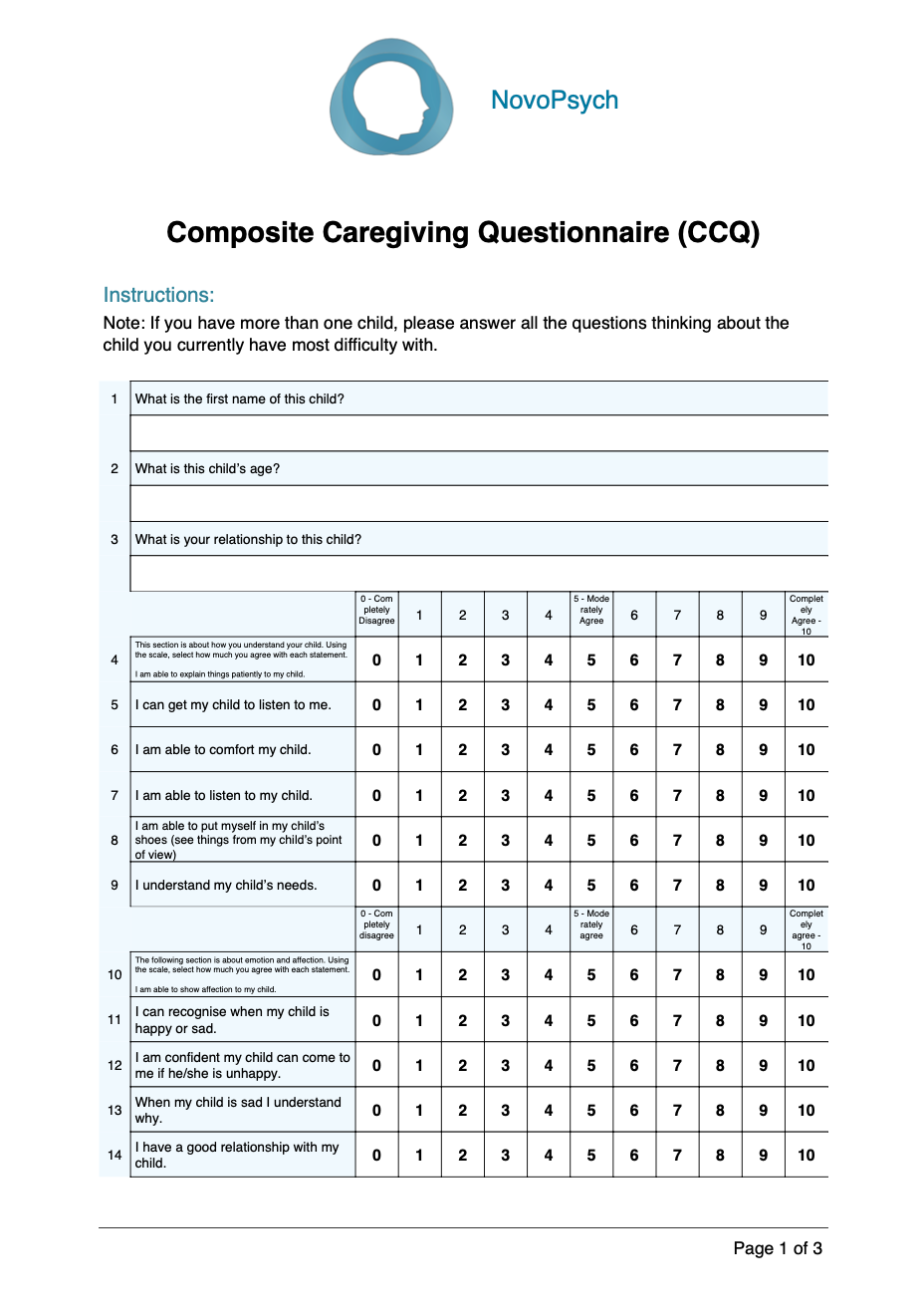
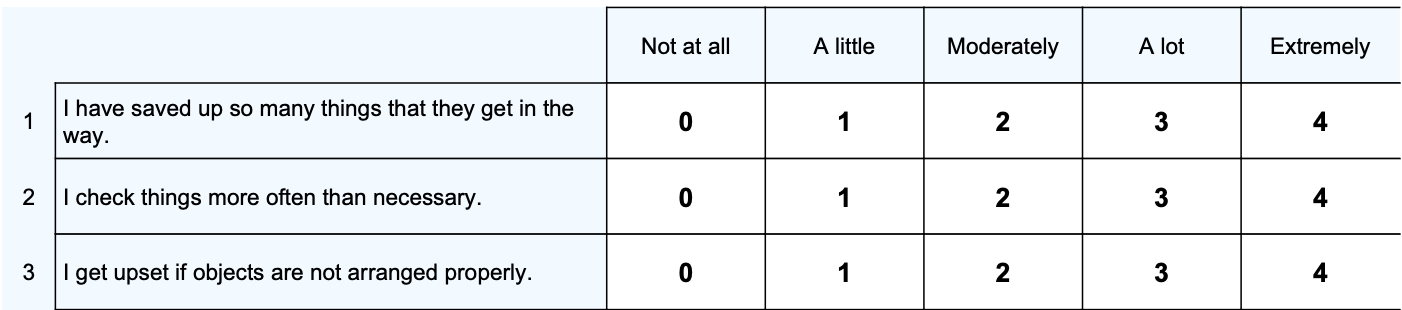
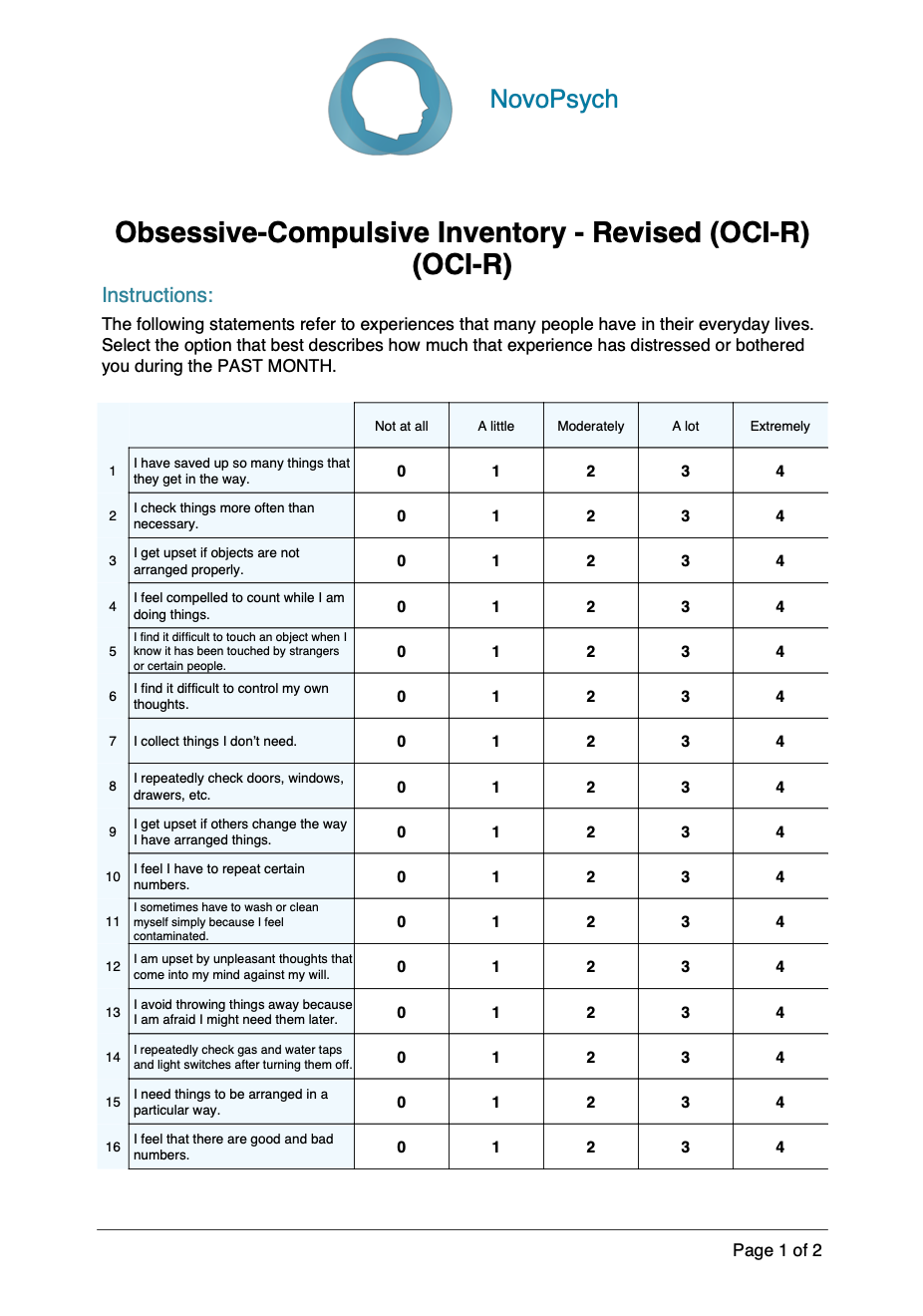
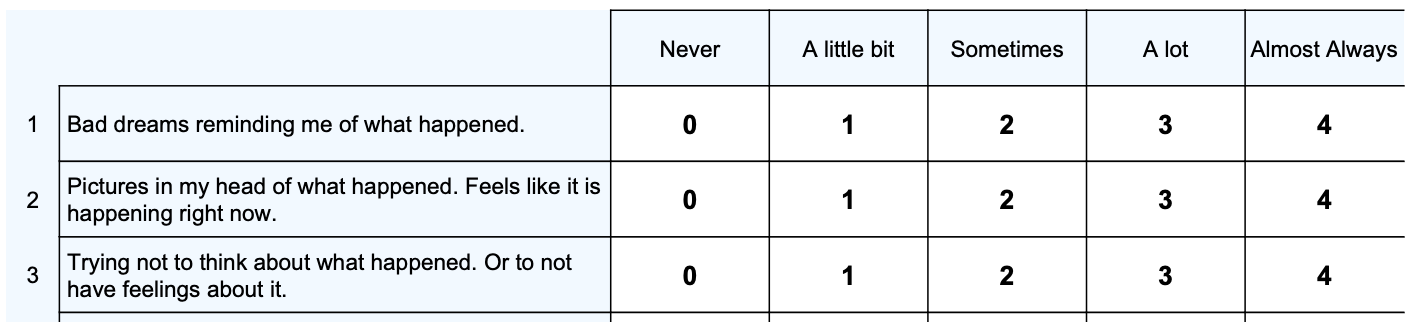
Example BEDSY Items:
For more information about the BEDSY, see the BEDSY website.
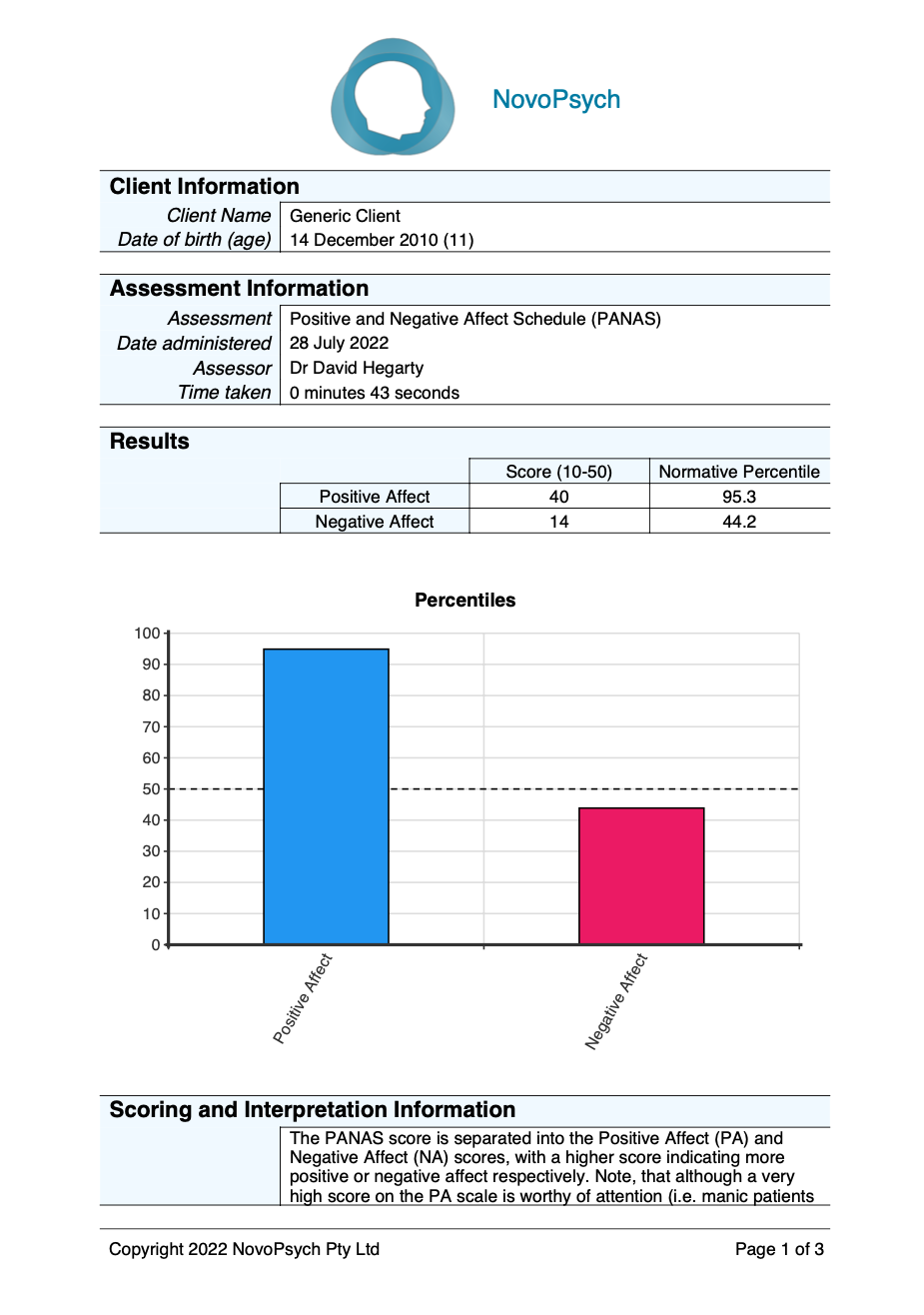
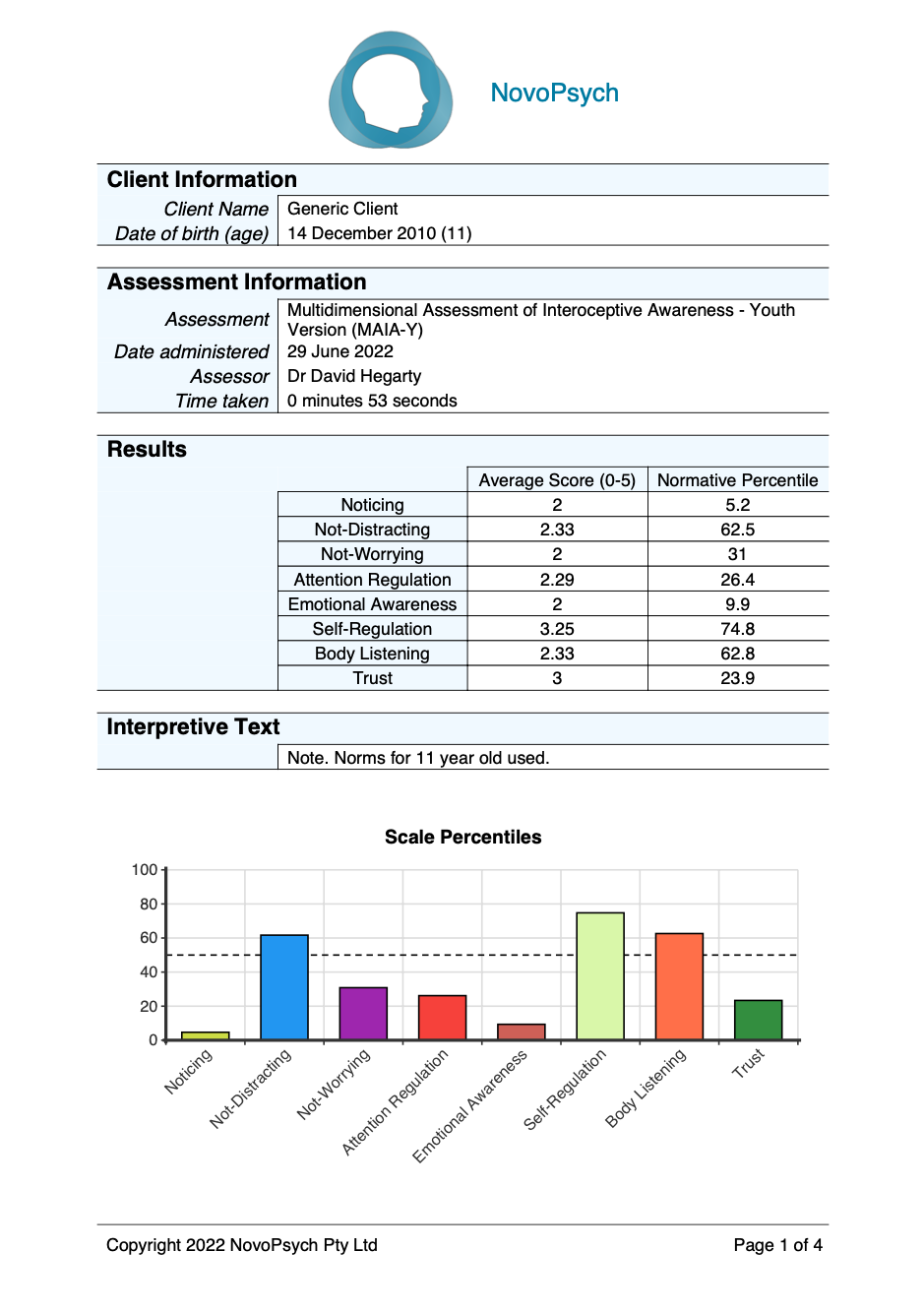
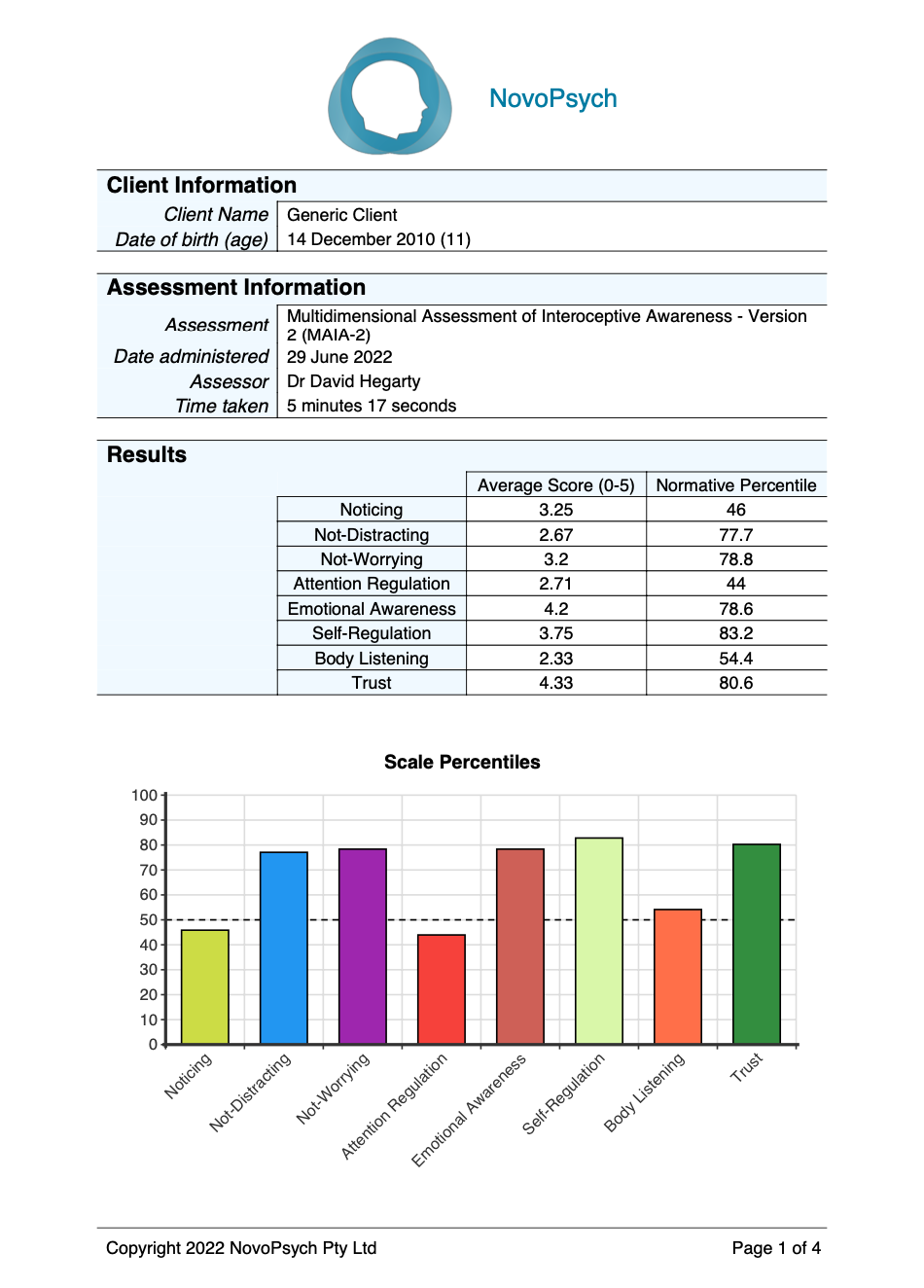
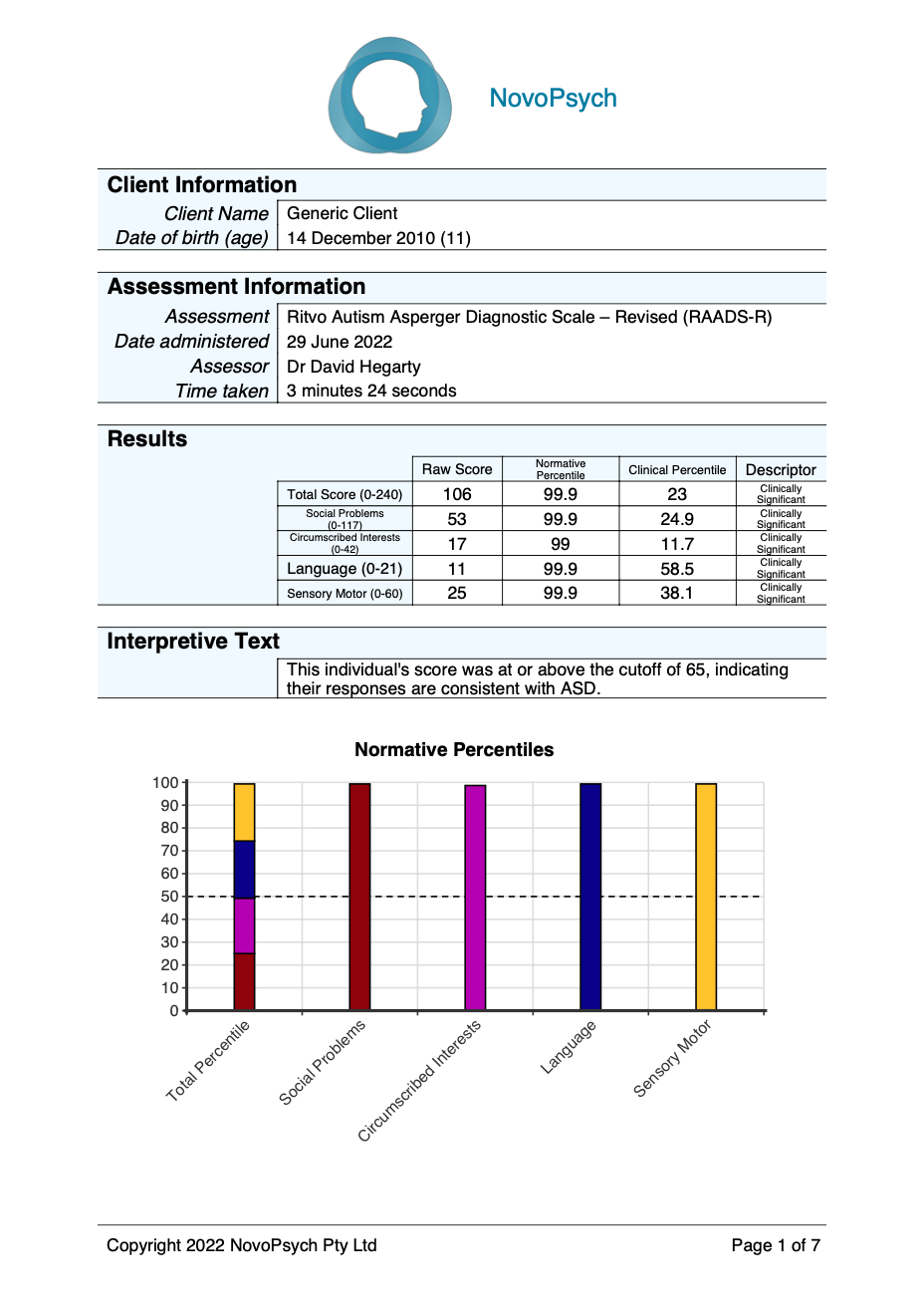
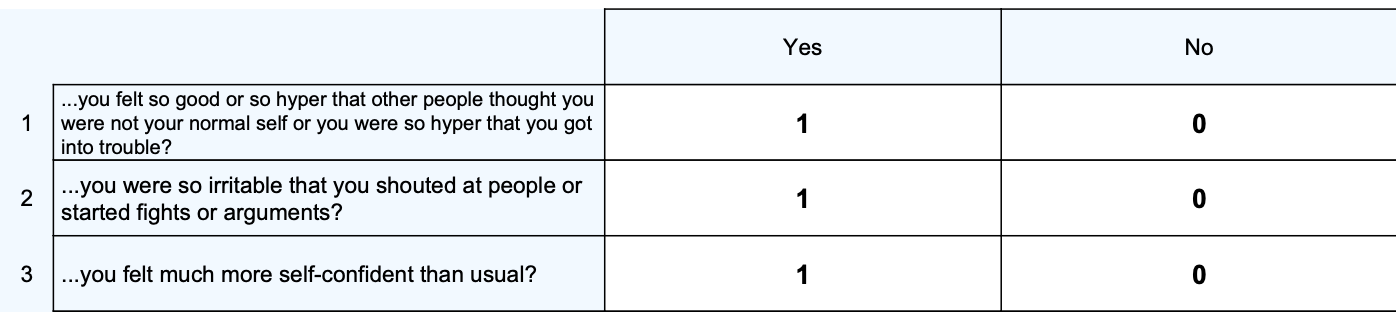
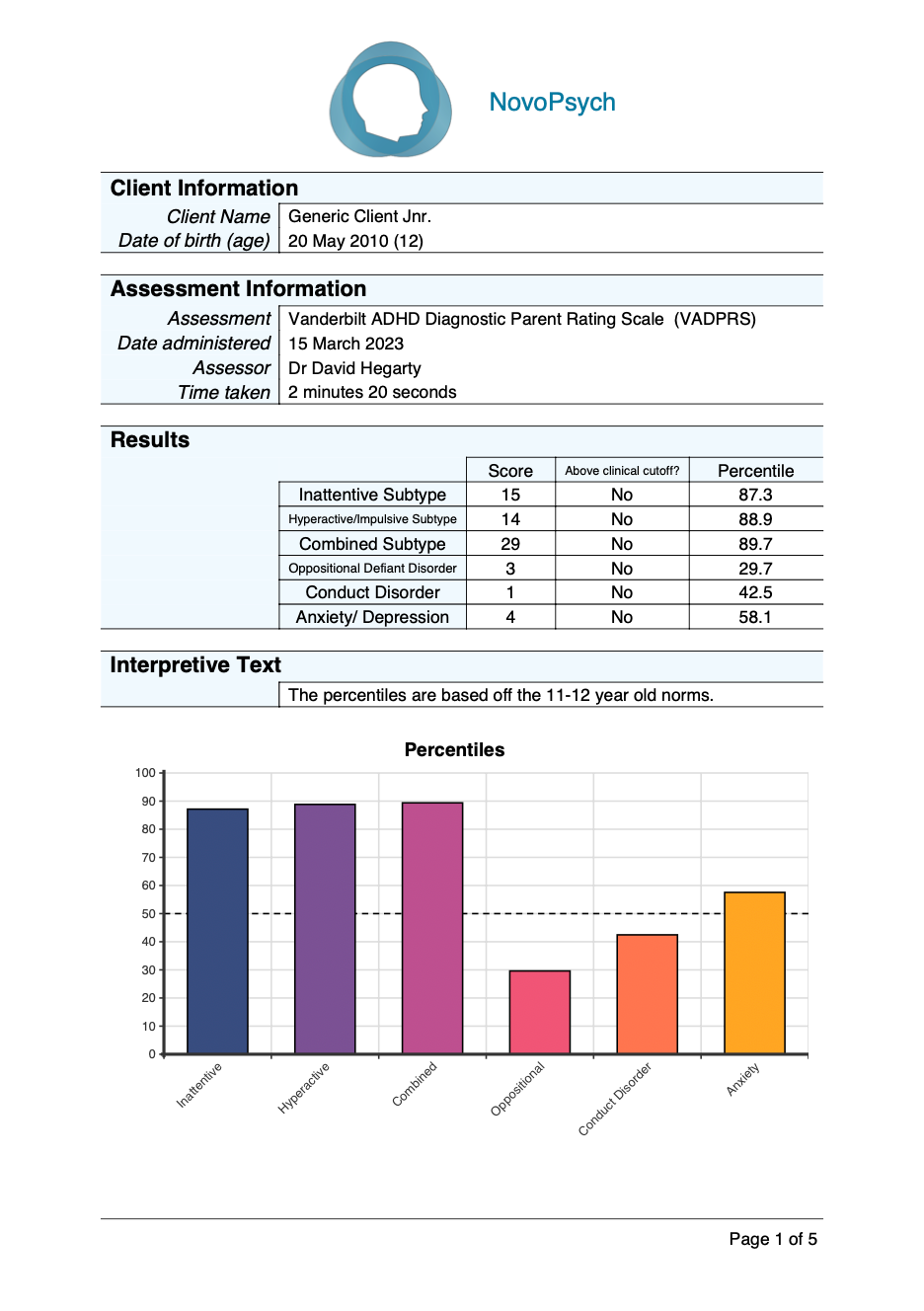
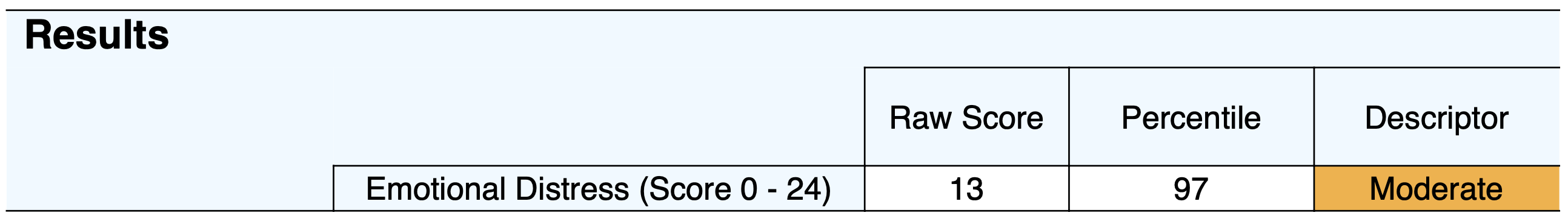
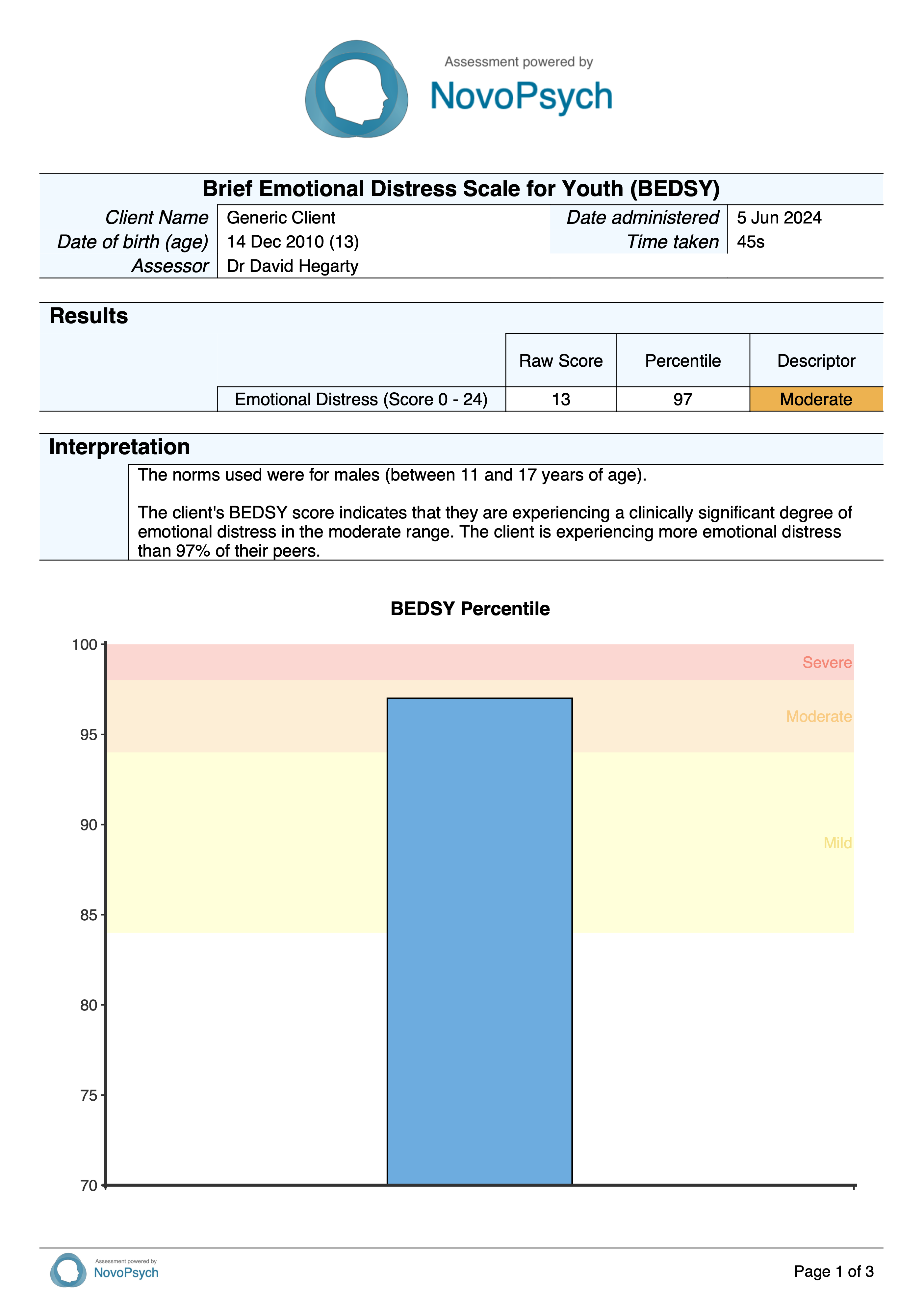
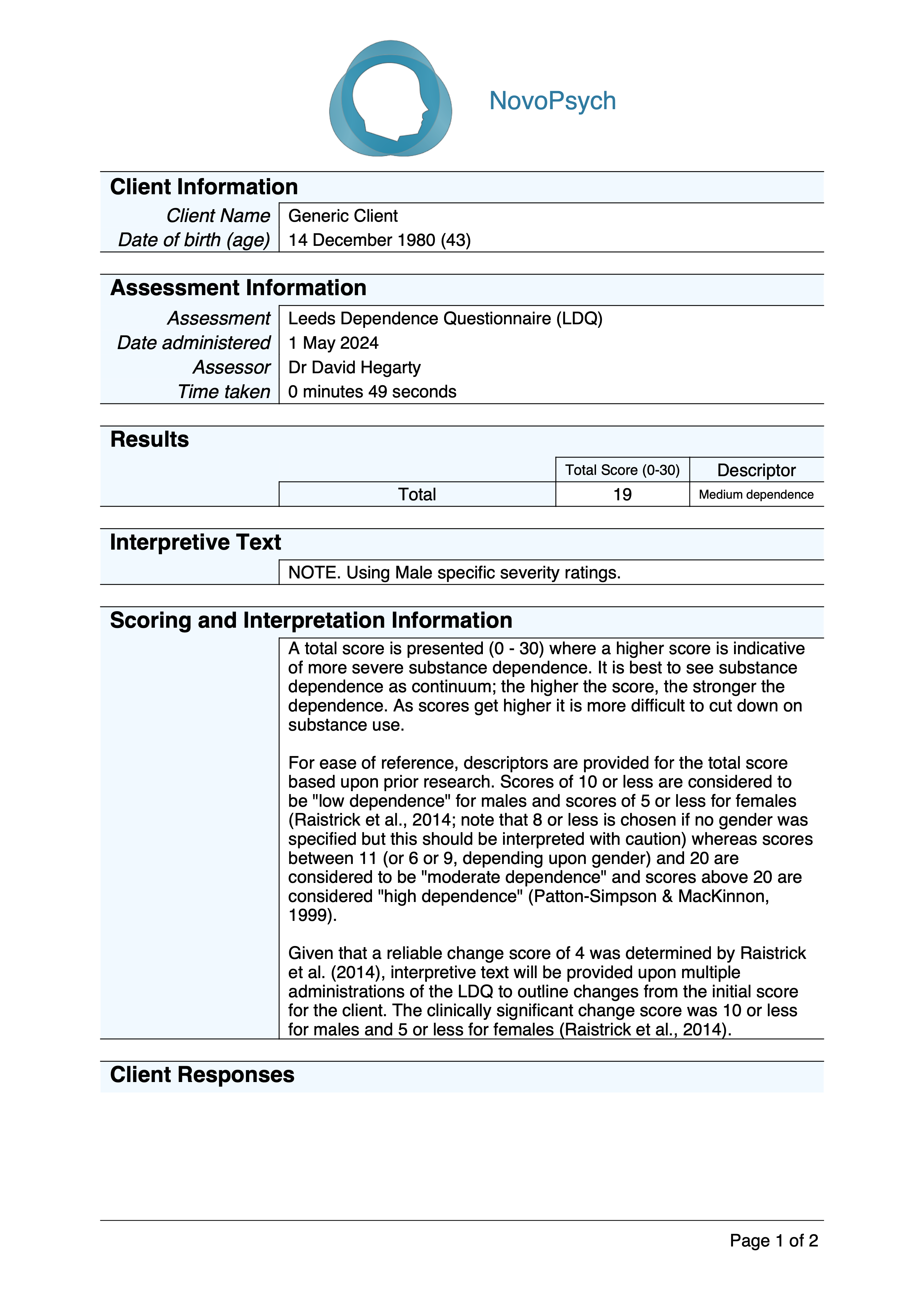
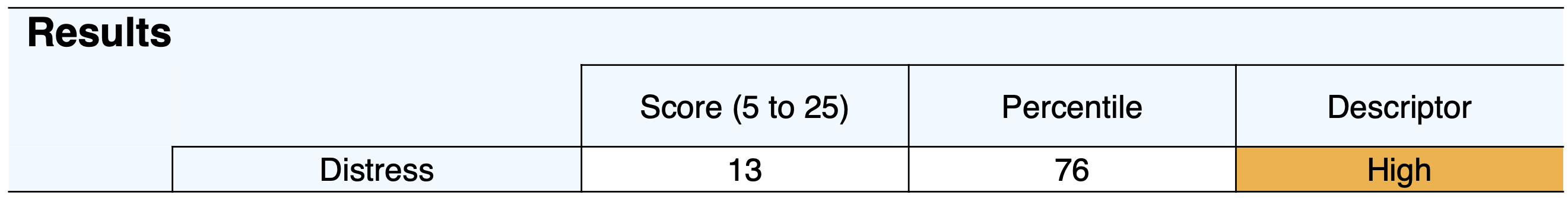
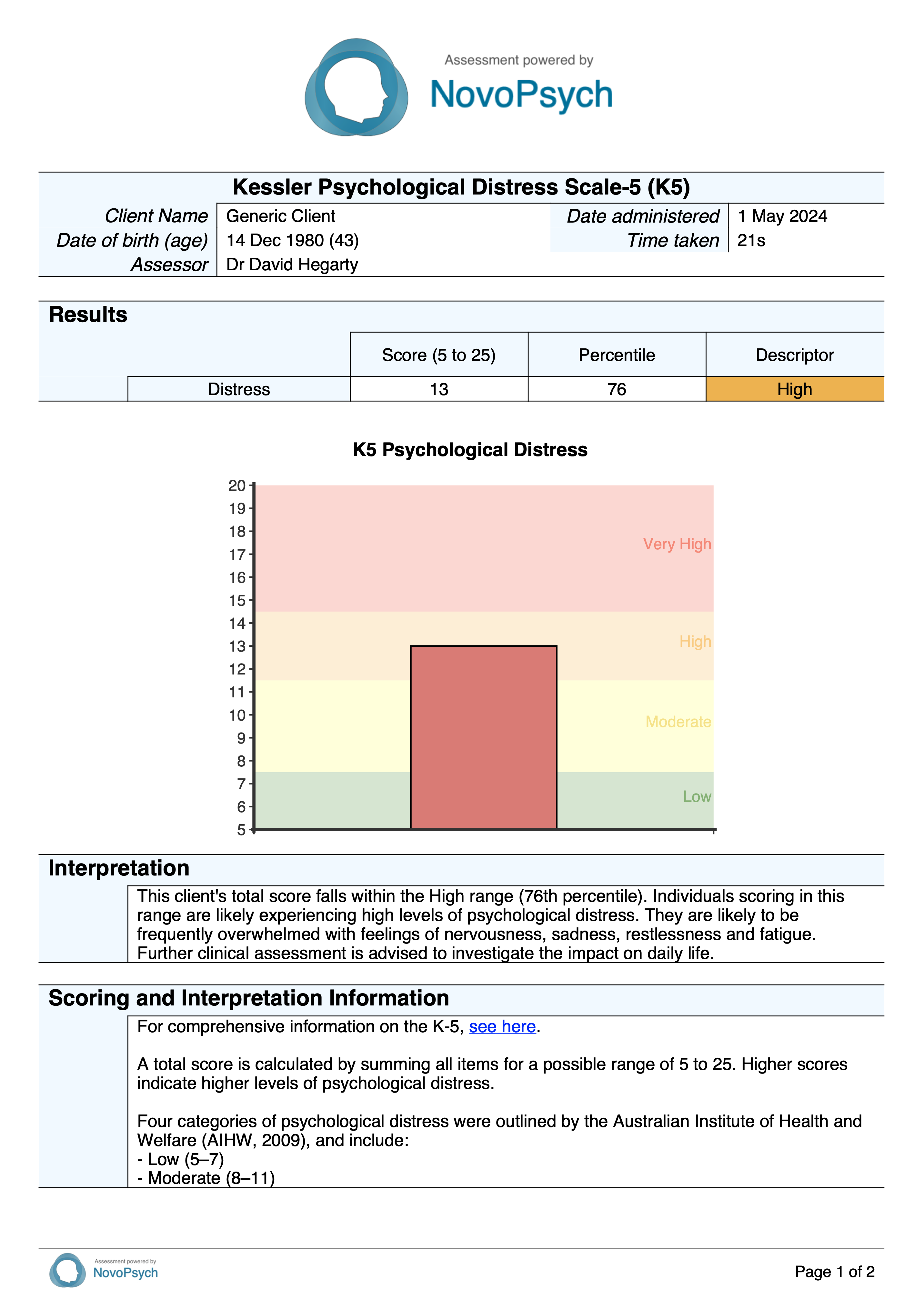
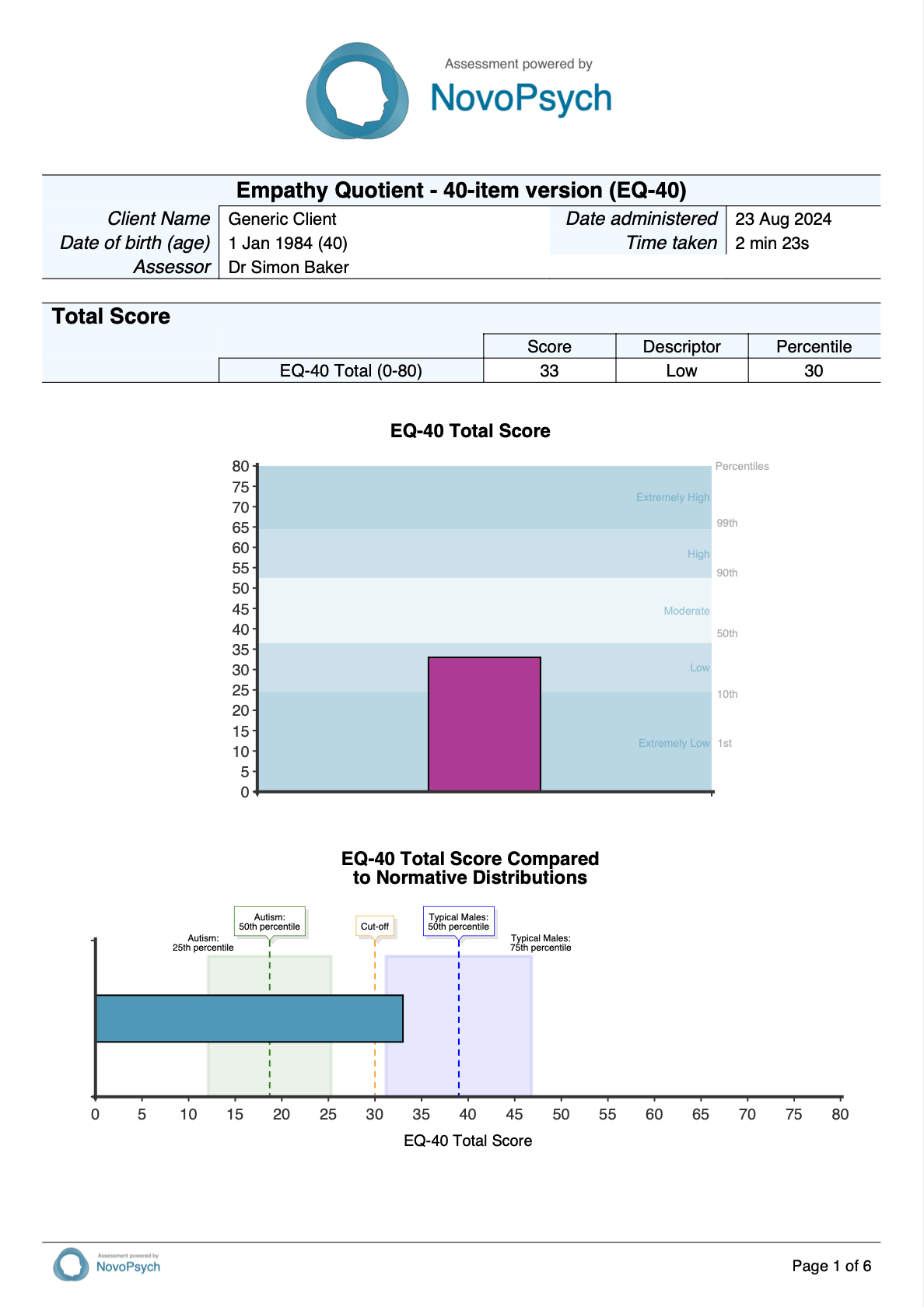
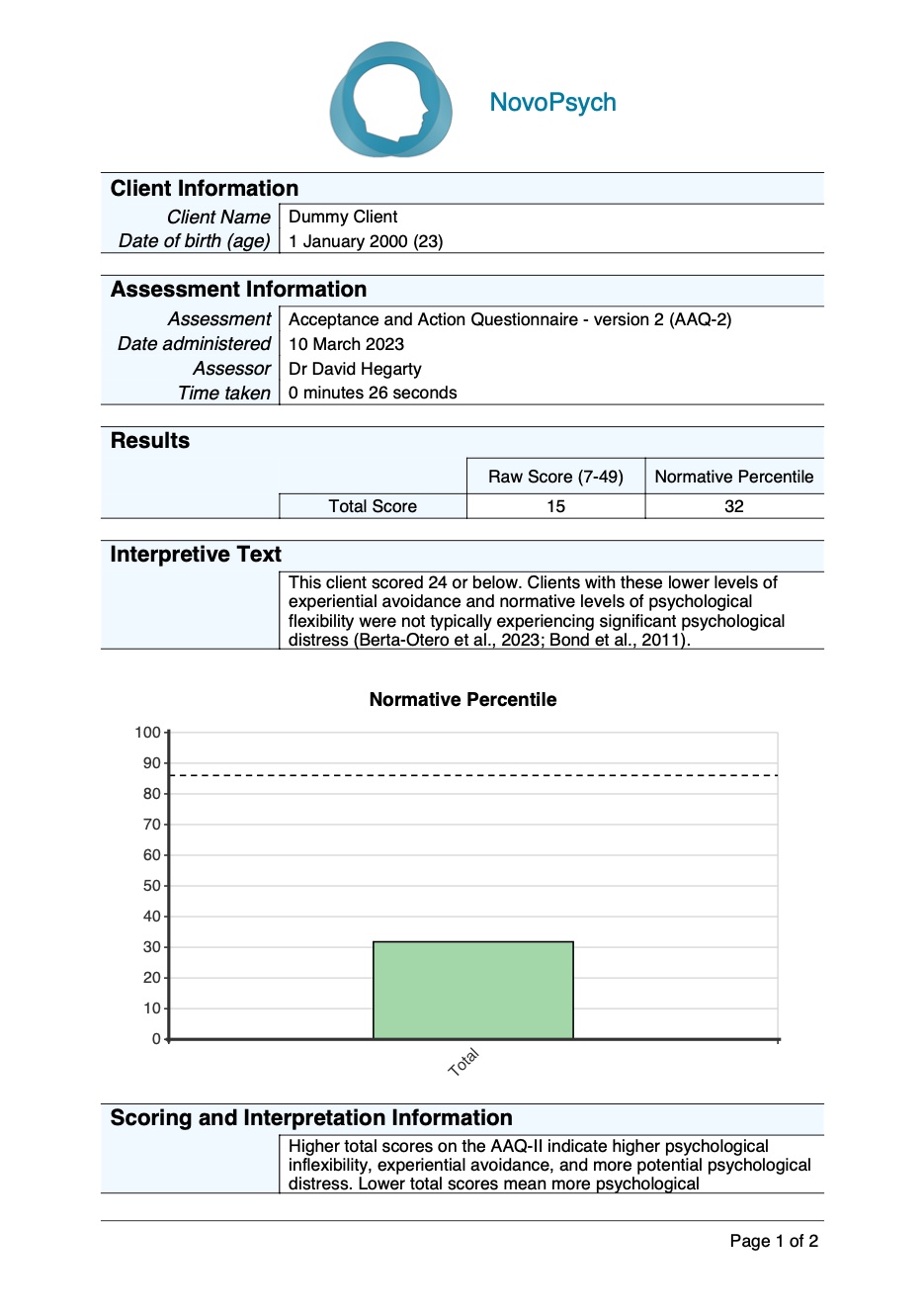
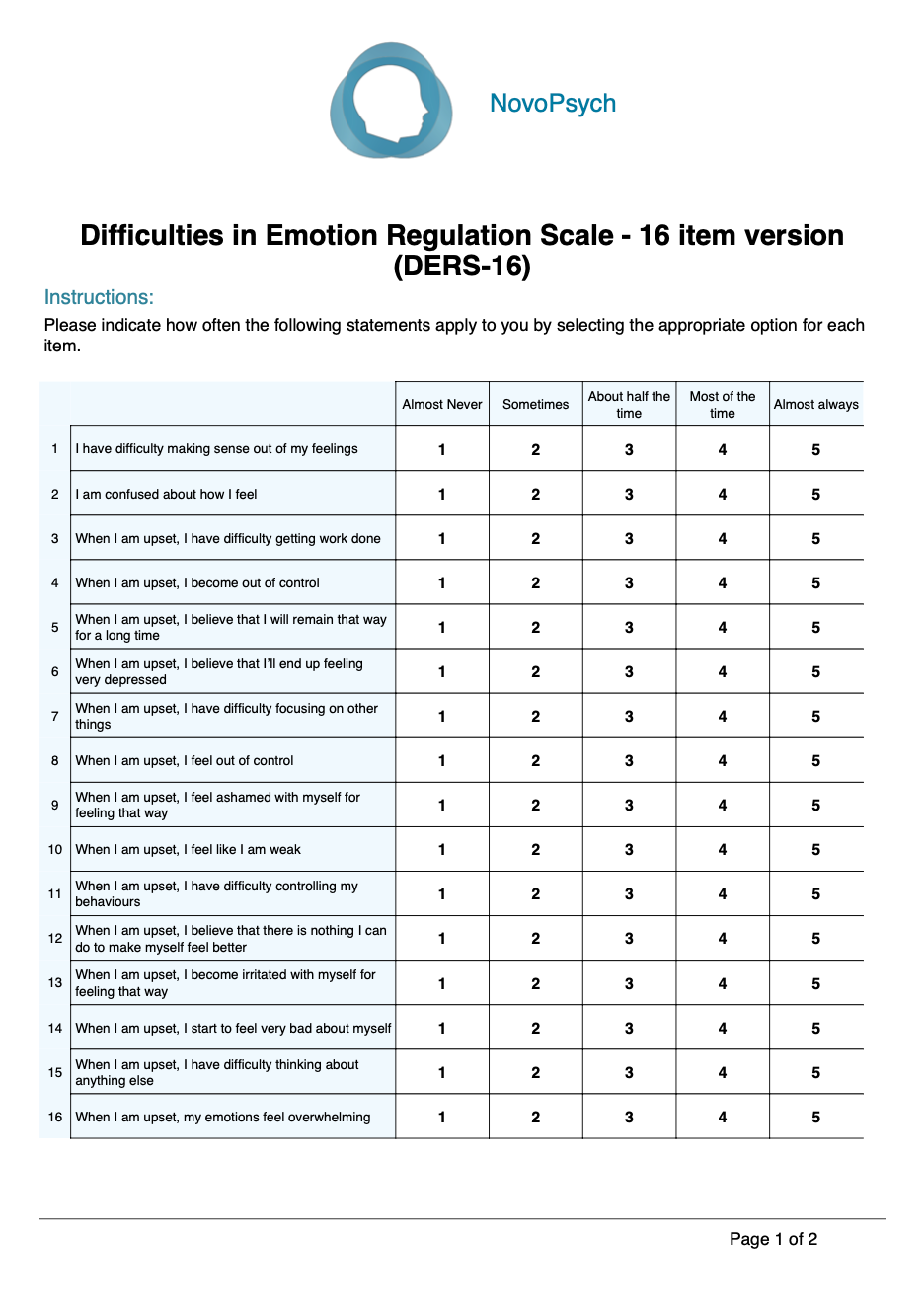
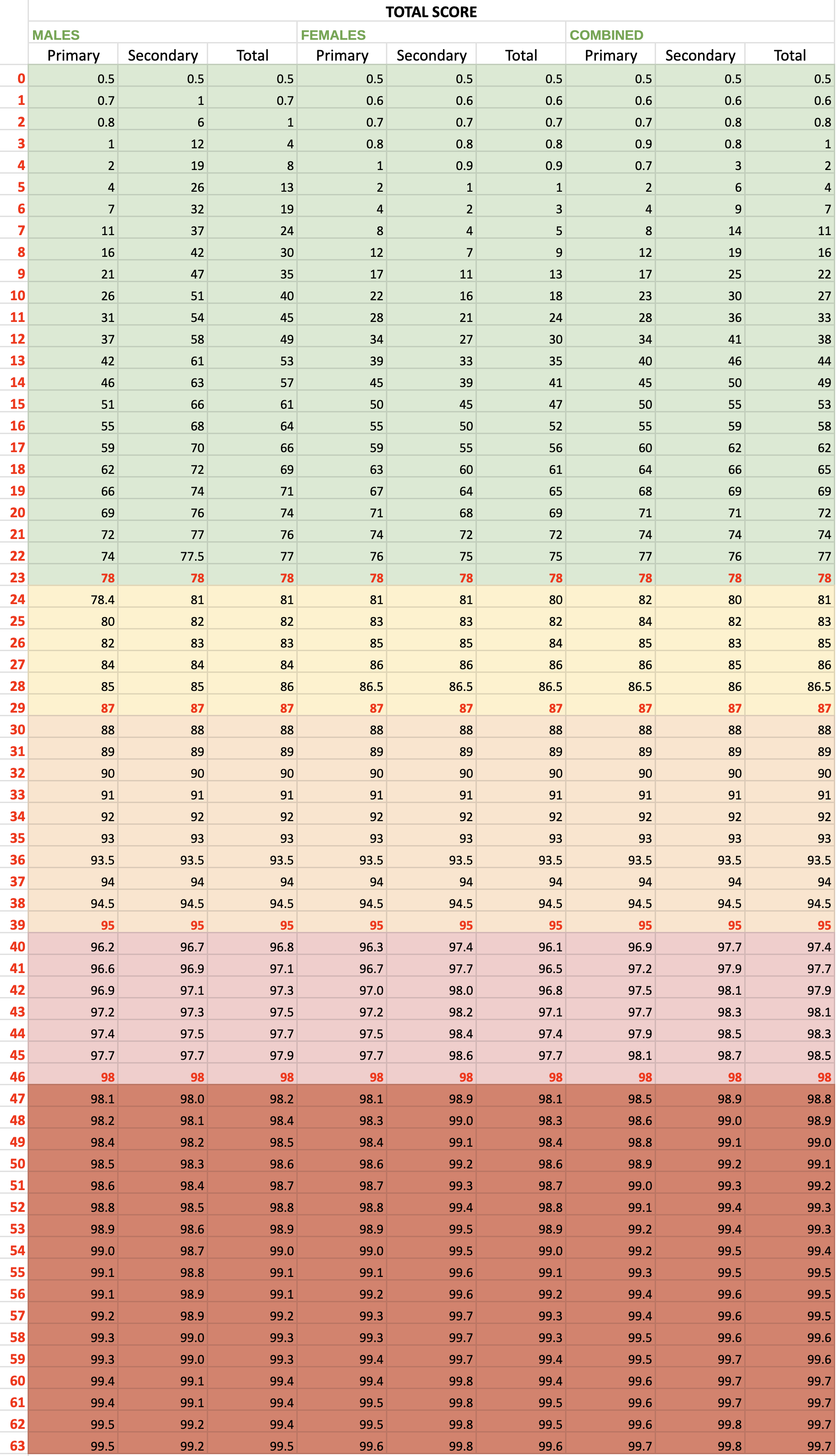
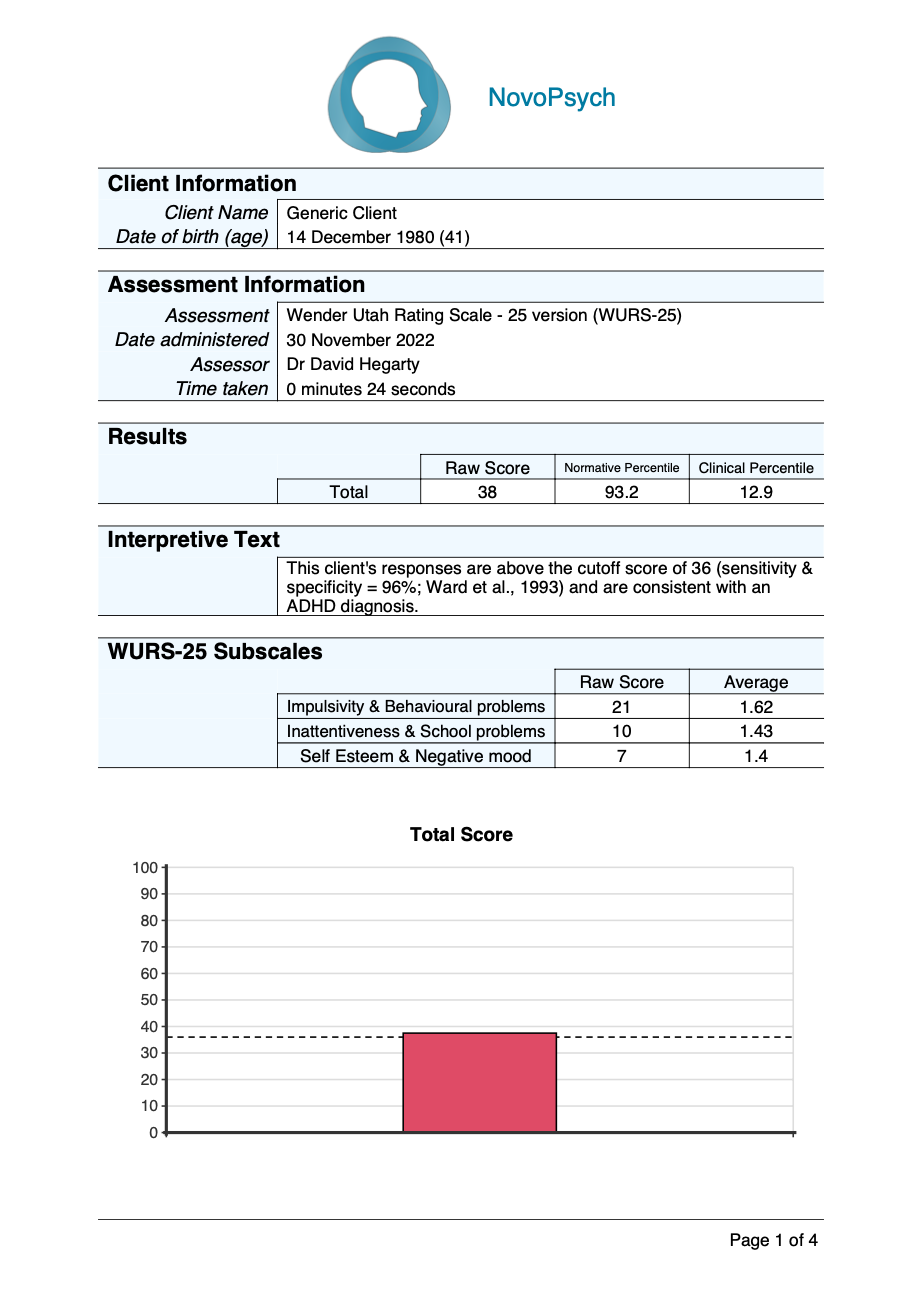
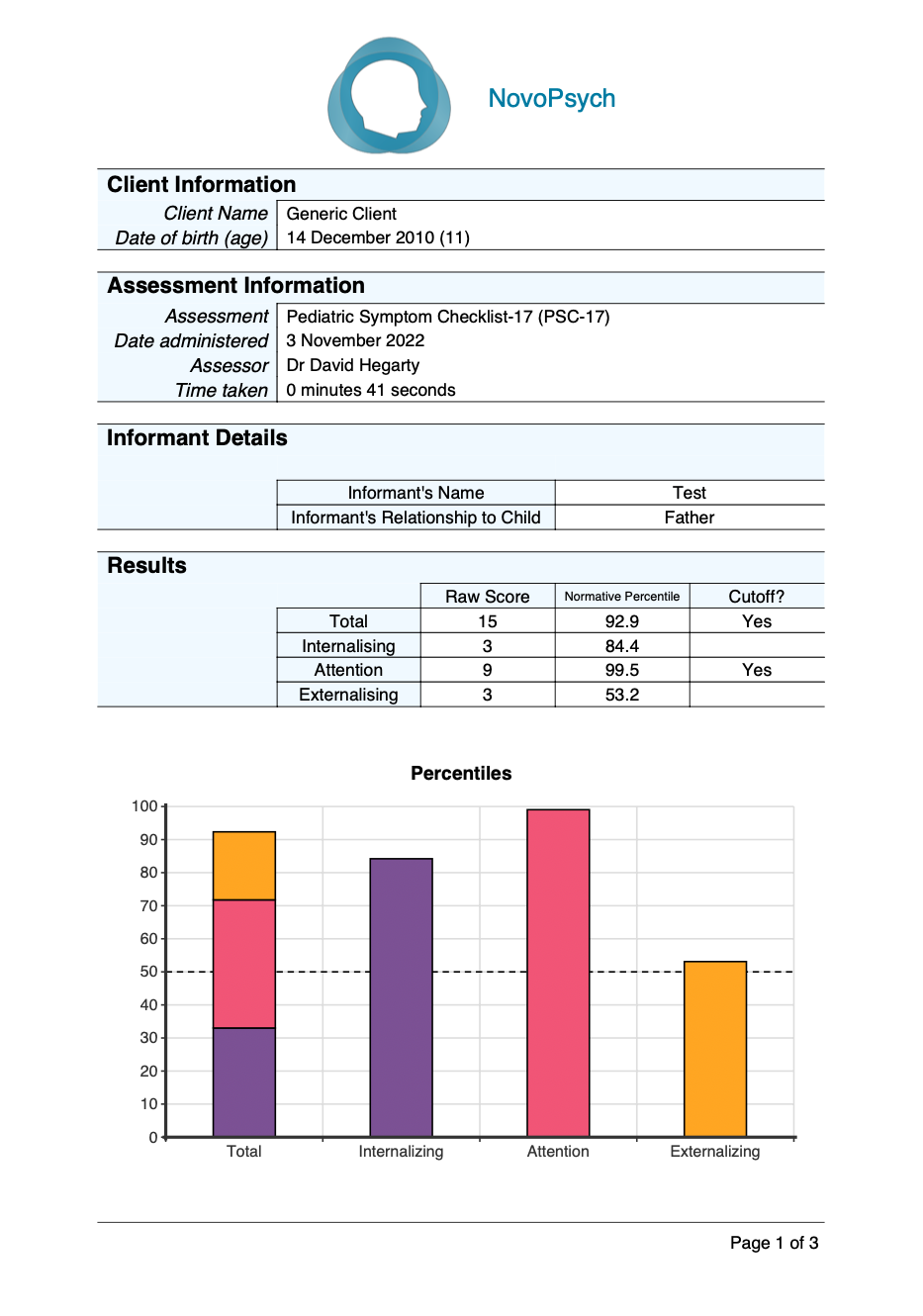
A total score is provided for the BEDSY (0 – 24) with higher scores indicating higher levels of emotional distress. In addition, percentiles are computed based on community samples and are dependent upon age brackets (11-17 for males, 11-13 or 14-17 for females) and gender (Spence & Rapee, 2022).
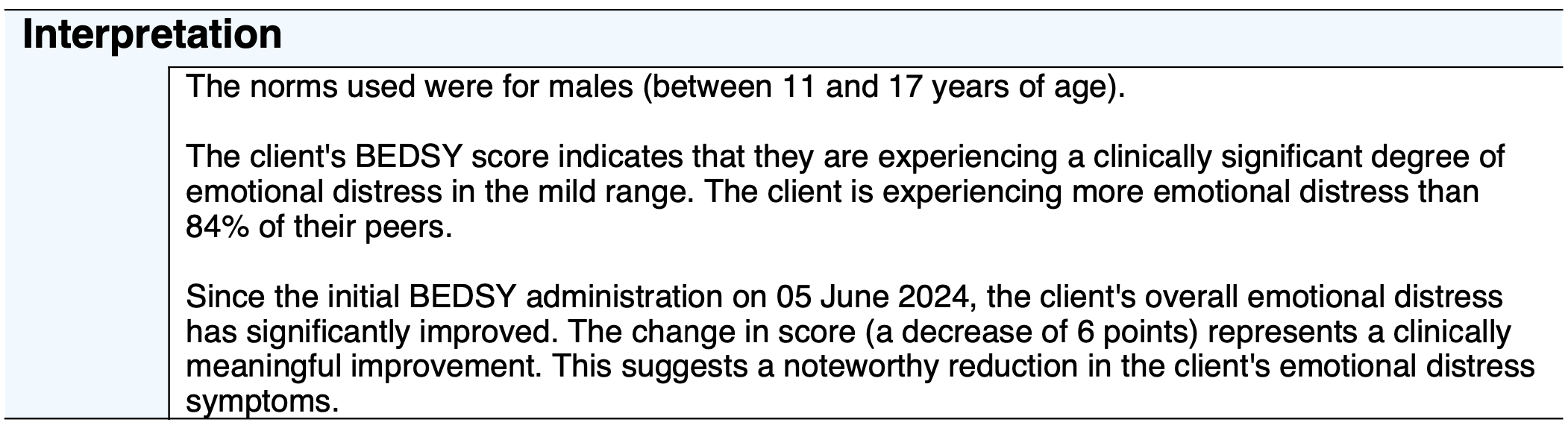
A percentile of 50 indicates an average and healthy level of emotional distress when compared to their age and gender-related peers. Note that females scored significantly higher on the BEDSY than males (Spence & Rapee, 2022), so the same score for each gender will give significantly different percentiles and, as a result, potentially different severity descriptors.
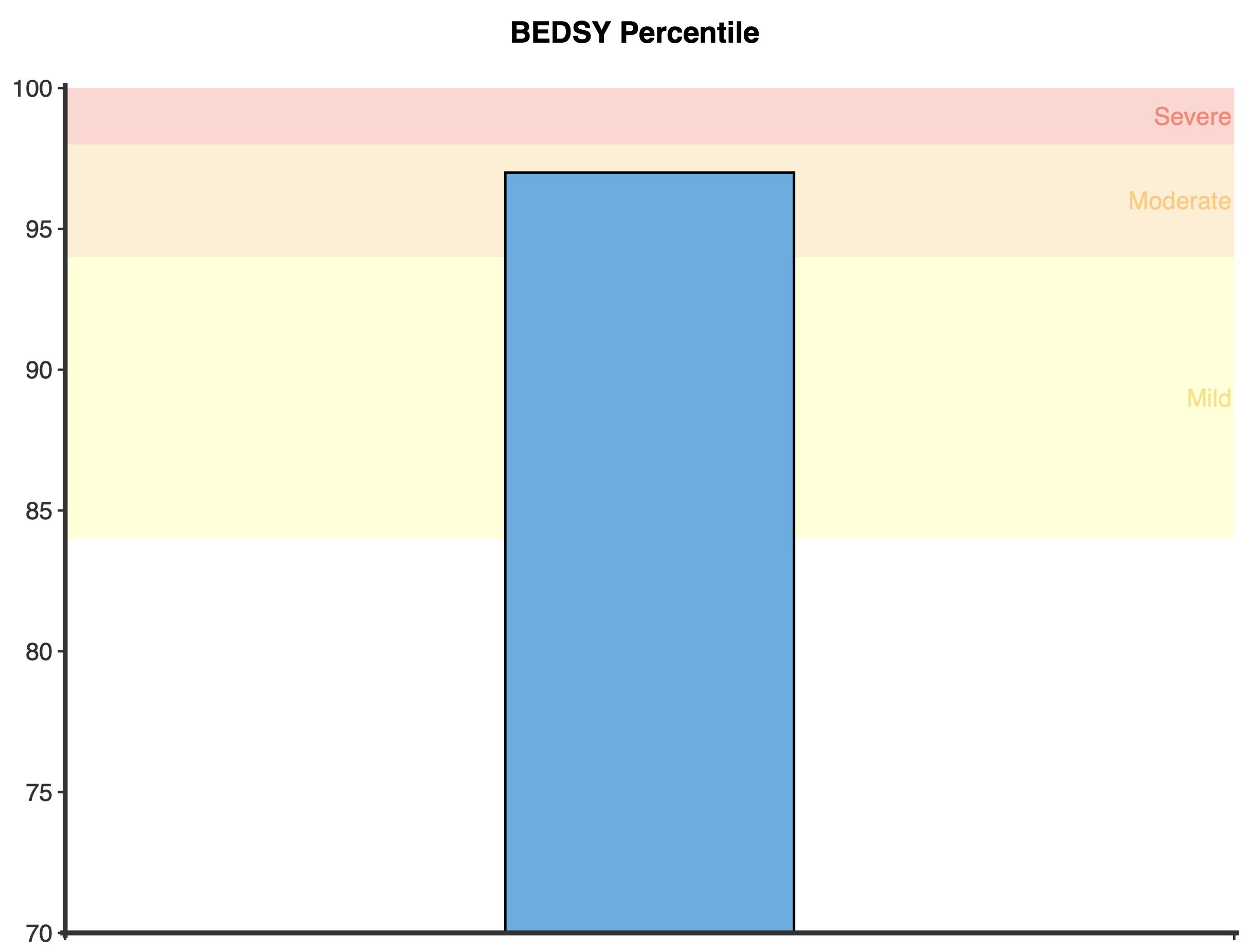
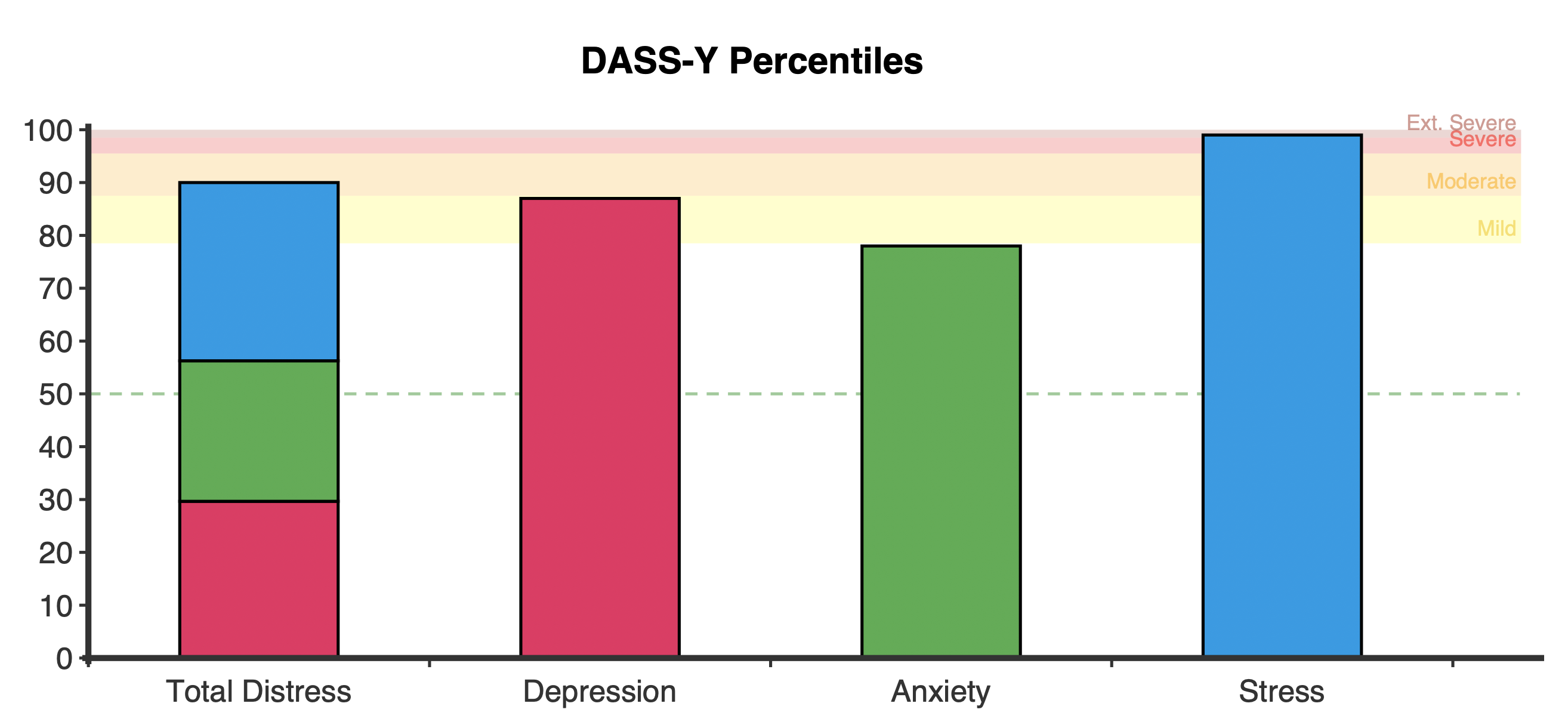
Scores are categorised into four severity ranges and are dependent upon the percentiles (S. H. Spence & R. M. Rapee, personal communication, May 1, 2024):
- Normal: Percentile of less than 84
- Mild: Percentile of 84 or greater and less than 94
- Moderate: Percentile of 94 or greater and less than 98
- Severe: Percentile of 98 or greater
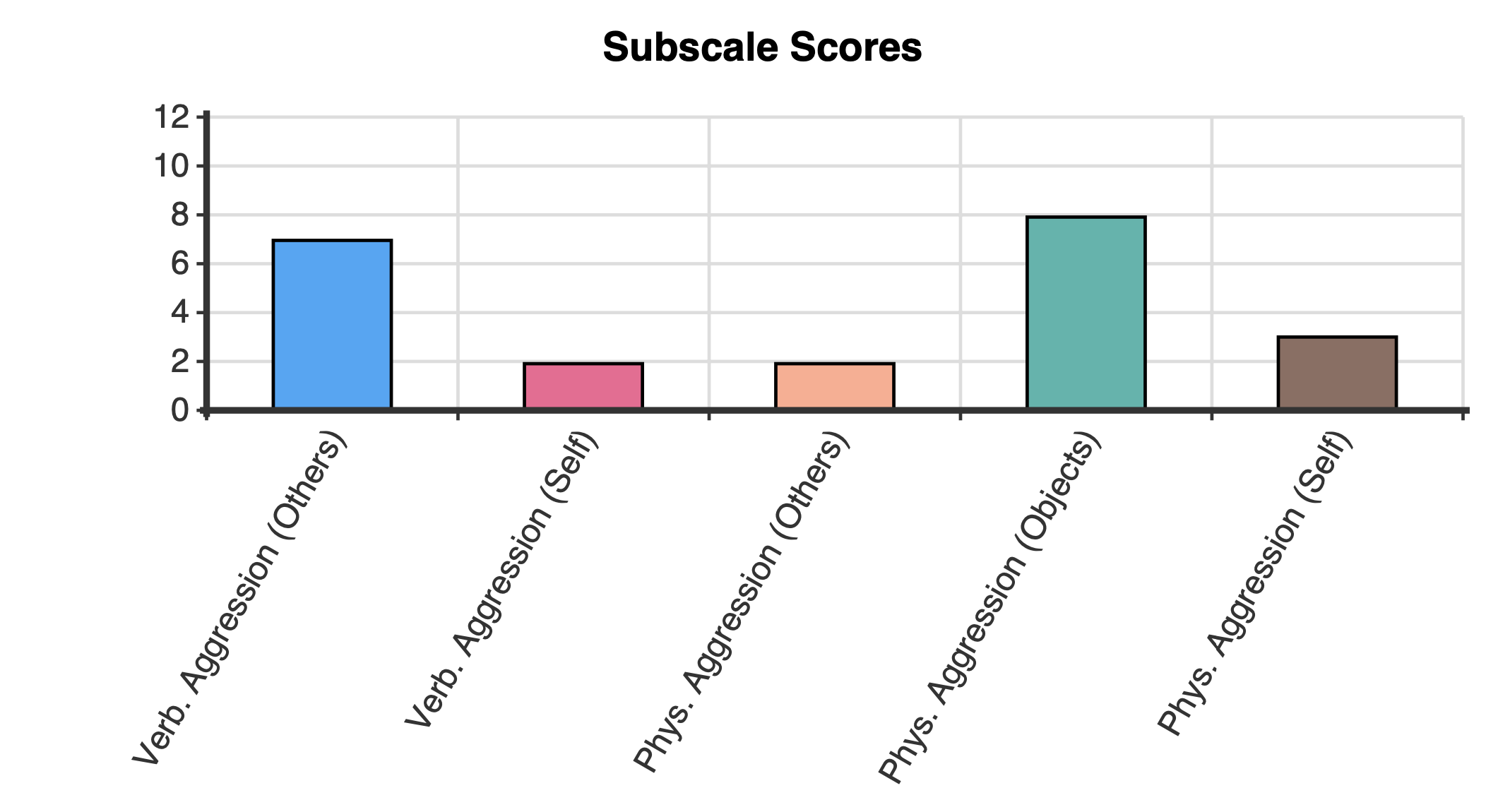
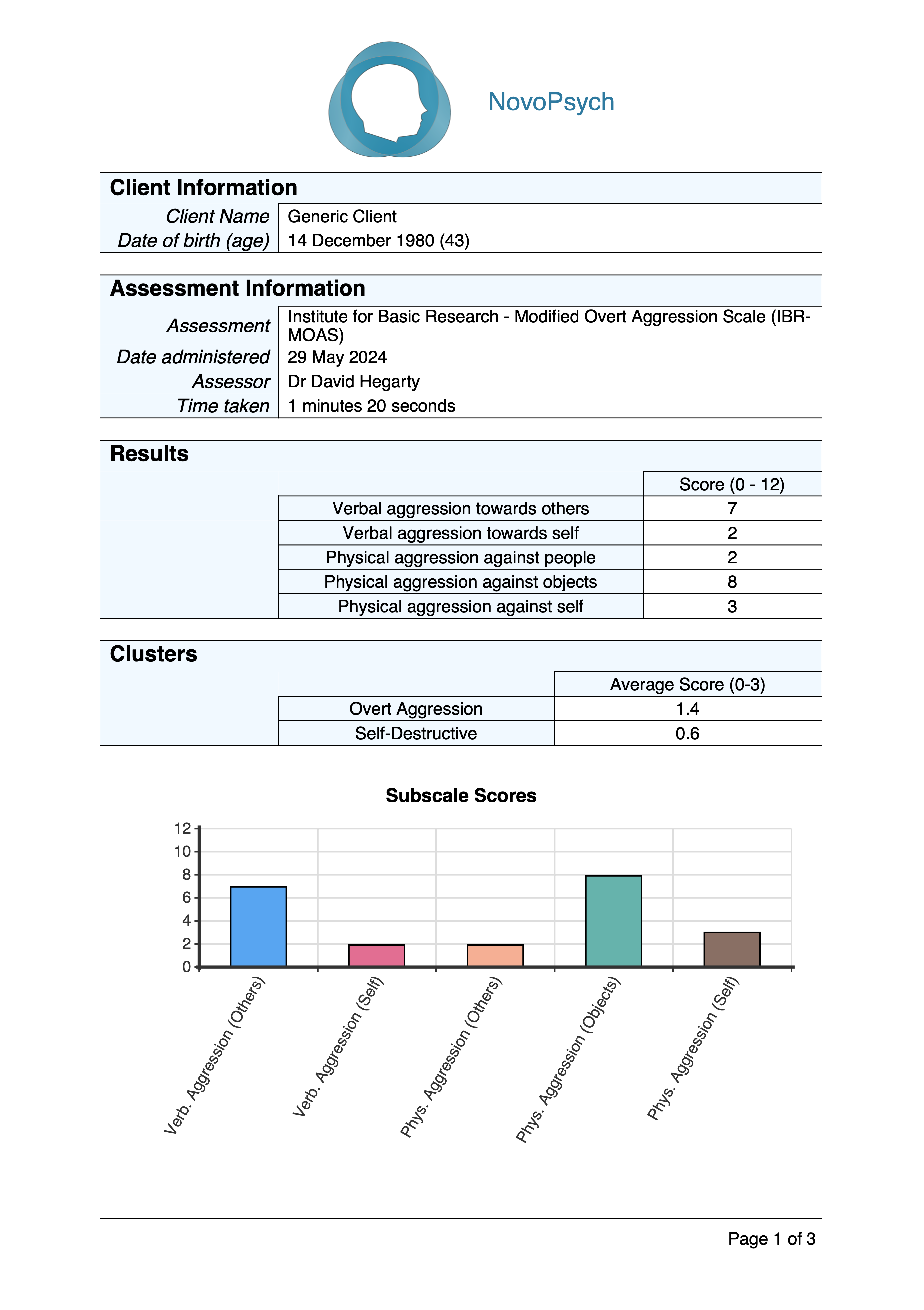
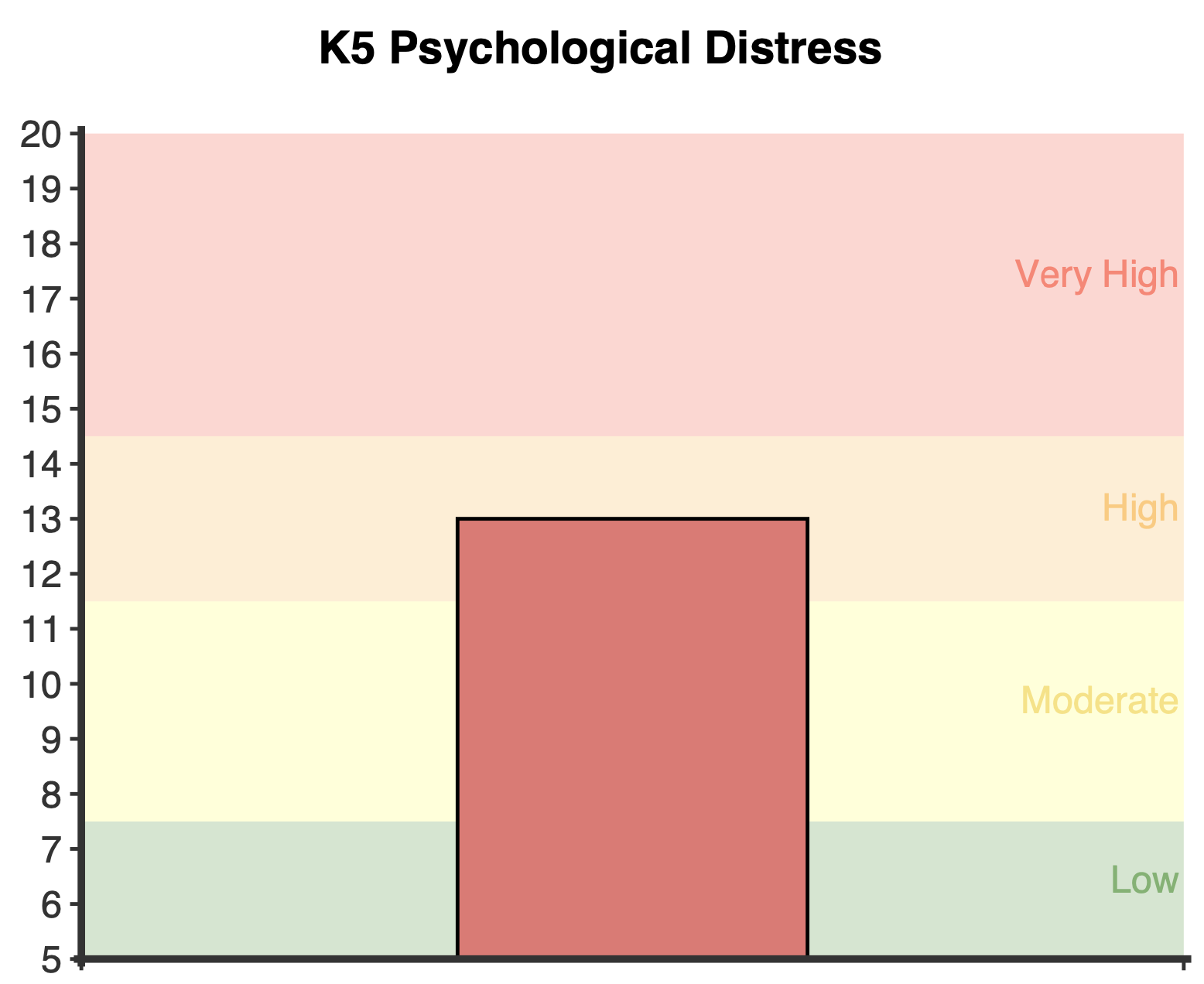
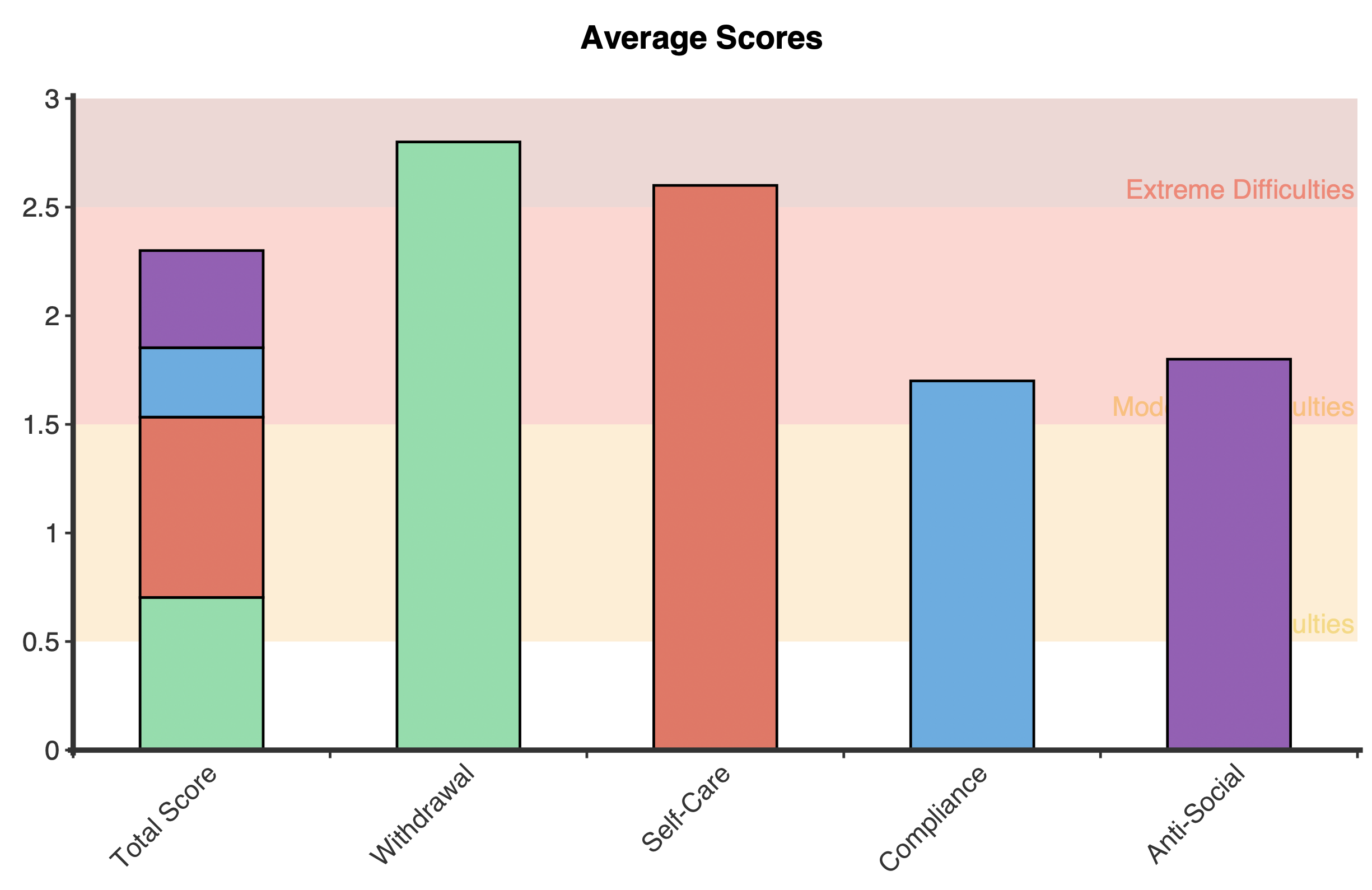
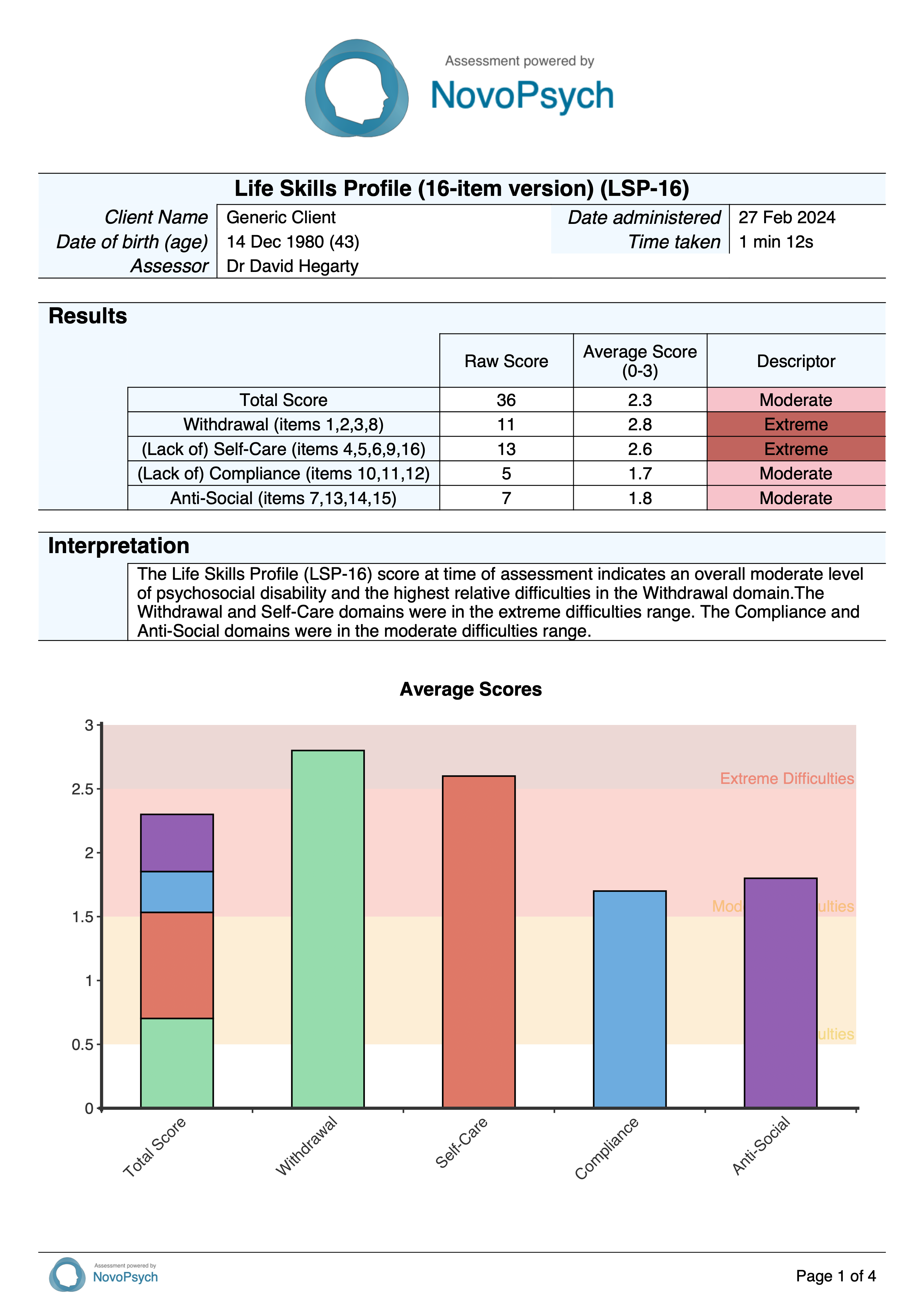
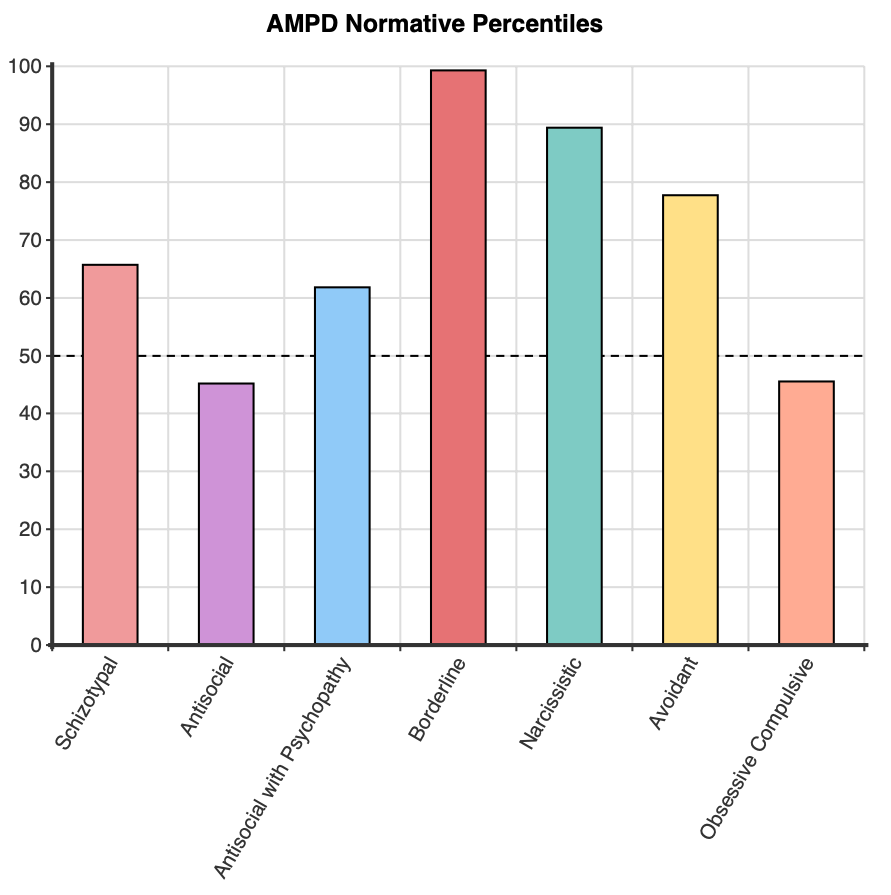
After the first administration, a plot is presented that shows the client’s percentile score with the severity ratings in the background.
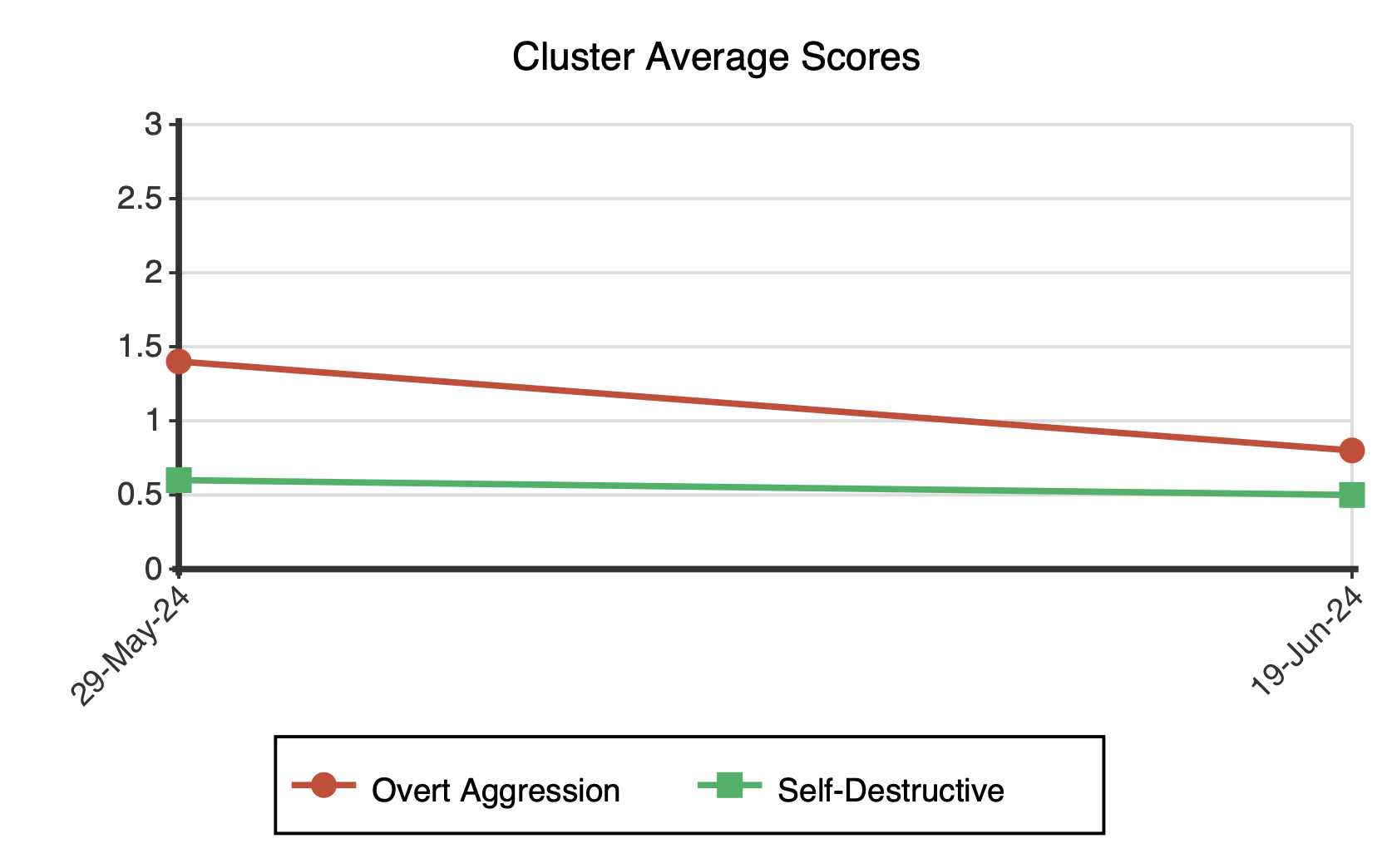
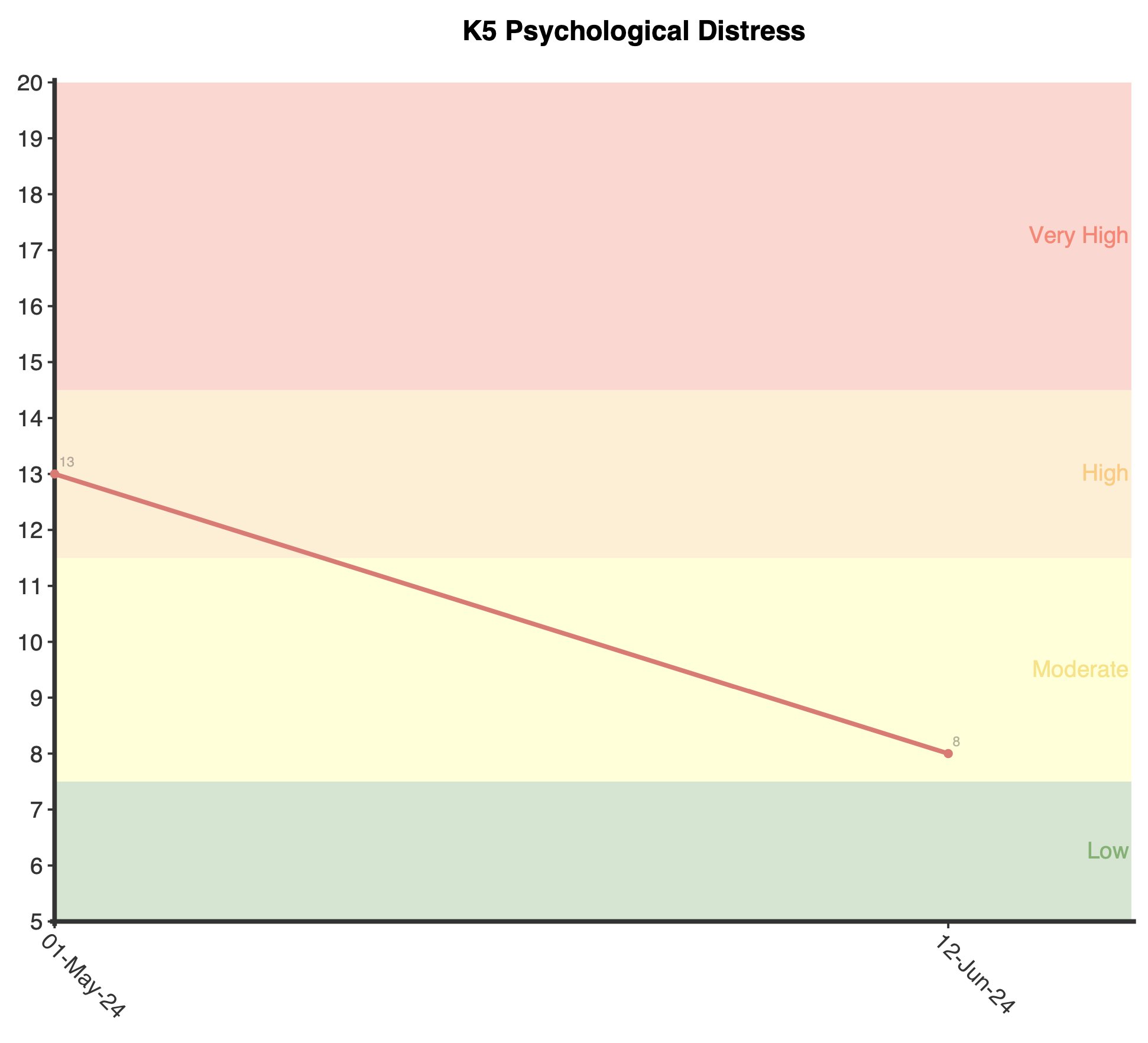
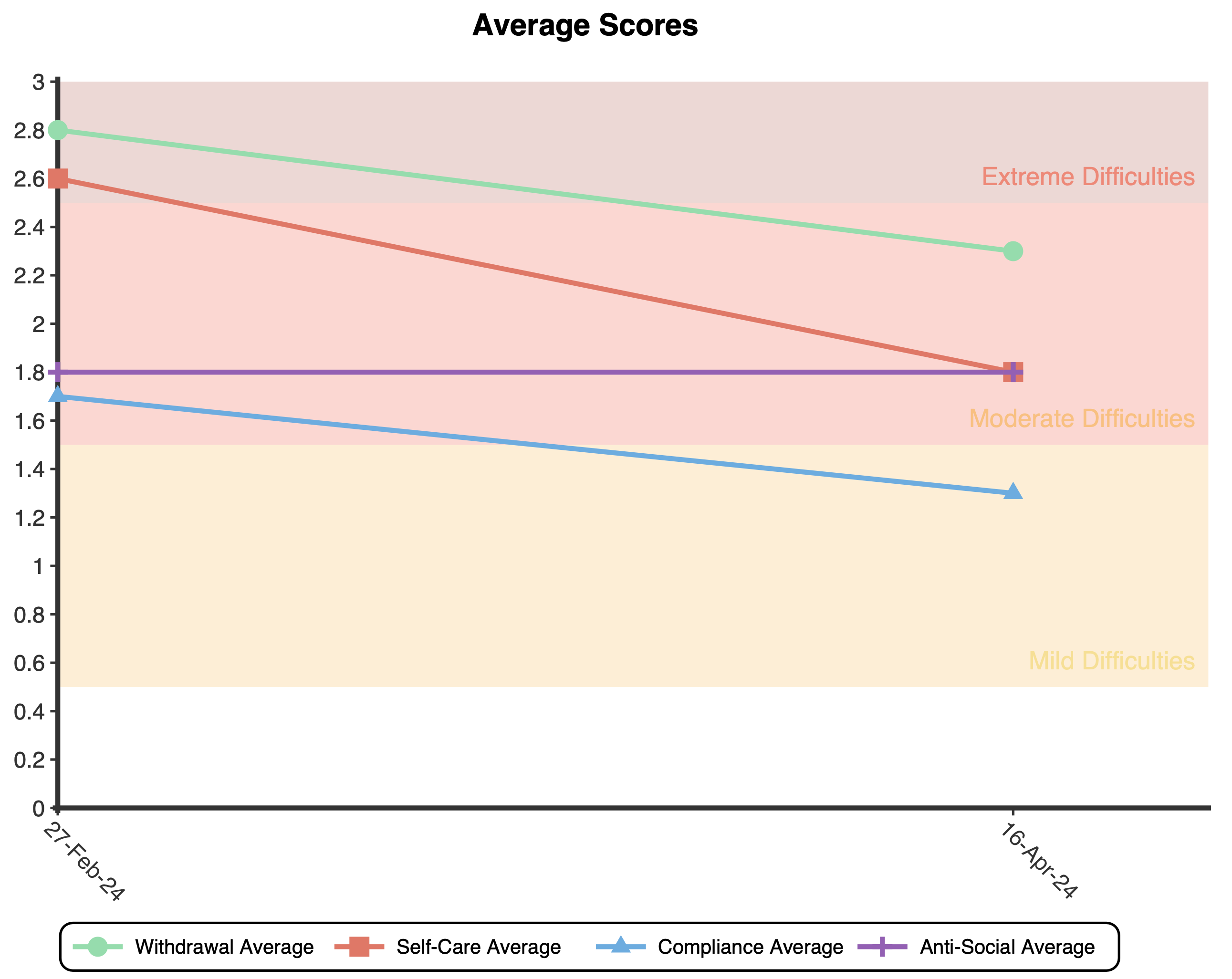
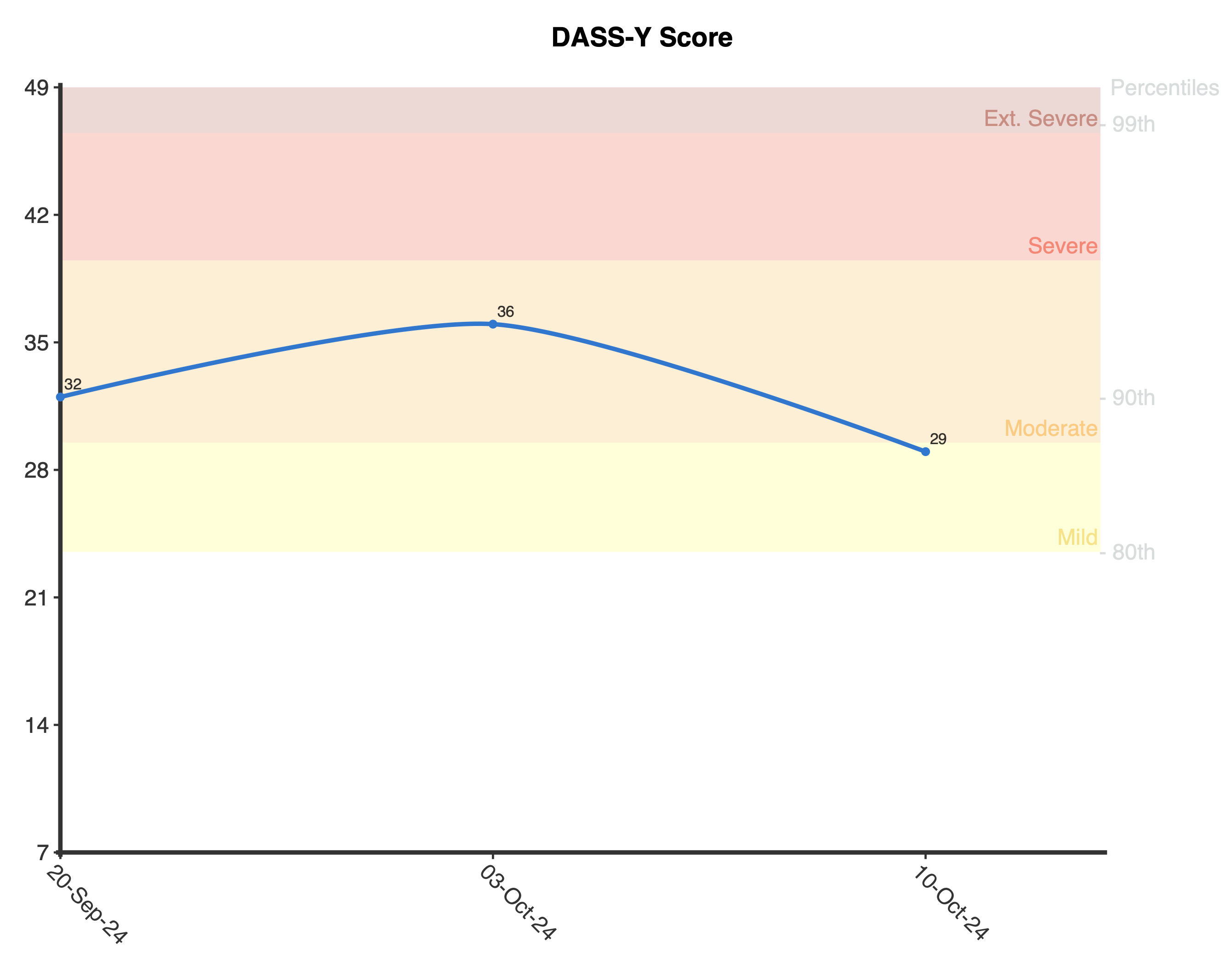
After multiple administrations a longitudinal plot will be displayed for the BEDSY total score over time.
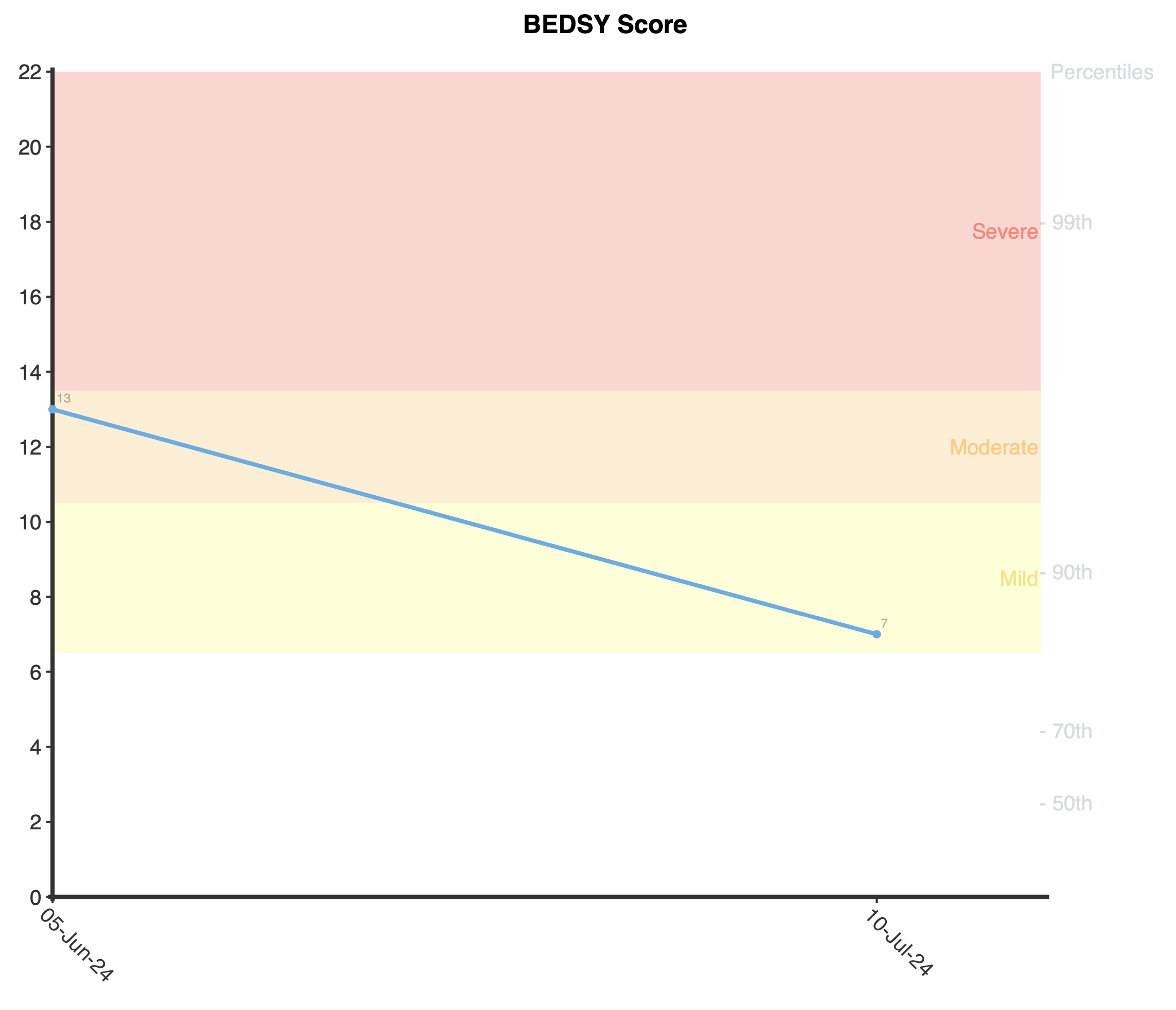
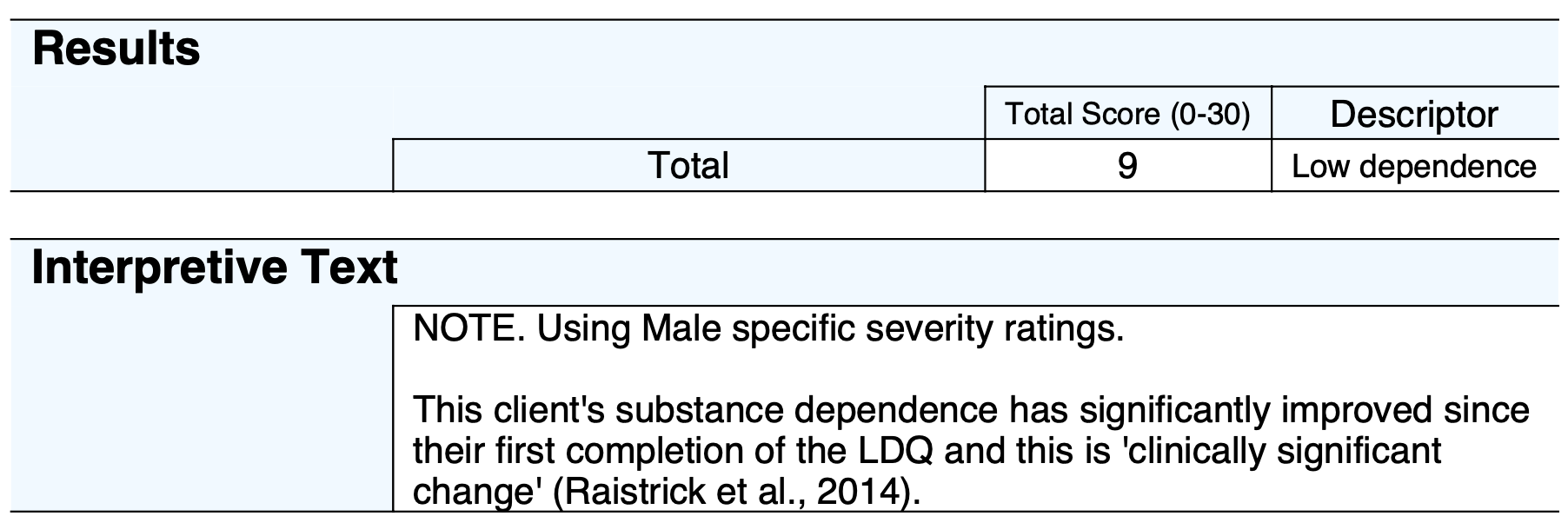
After multiple administrations, interpretive text will be provided that will outline if the change in score is clinically meaningful or not. This is based upon the Minimally Important Difference (MID; Norman, Sloan & Wyrwich, 2003) between the initial score on the BEDSY and the latest administration. The threshold score for clinically significant change is 2 points or more.
Example BEDSY Interpretive Text:
As the BEDSY has displayed strong internal consistency, good construct validity, and acceptable discrimination between clinical and non-clinical samples.
The BEDSY was initially developed using a sample of 2,663 school students (aged 11-17; 48.8% boys, 50.8% girls), with the items of the questionnaire checked for validity against a high depression symptom sample and an anxious referred sample (Spence & Rapee, 2022). The scale was shortened from 20 to 8 items using confirmatory factor analysis (CFA) and Item Response Theory (IRT), and had strong internal consistency (Cronbach’s α = .88). The CFA suggested that the BEDSY has a bi-factor structure, with all items loading strongly on a general factor (.60, -.91) and weaker loadings on specific factors (i.e., depression and anxiety). As a result, it was determined that the BEDSY is a measure of emotional distress as opposed to measuring depression and anxiety separately.
The scale displayed sufficient construct validity as individuals who surpassed the clinical cut-off for depression on the Short Mood and Feelings Questionnaire (SMFQ) showed significantly higher total scores on the BEDSY compared to those who did not and with a large effect size (d = 2.55).
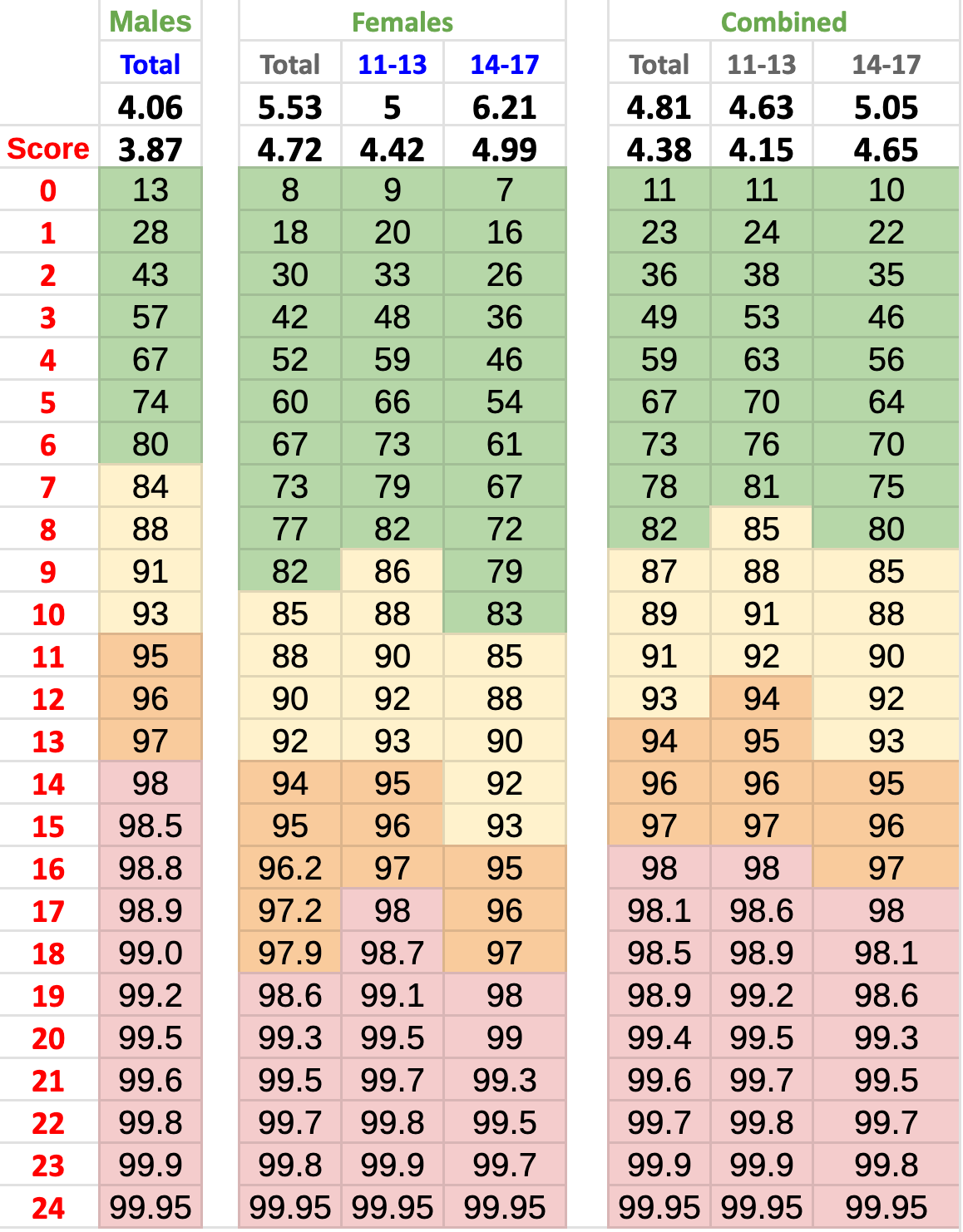
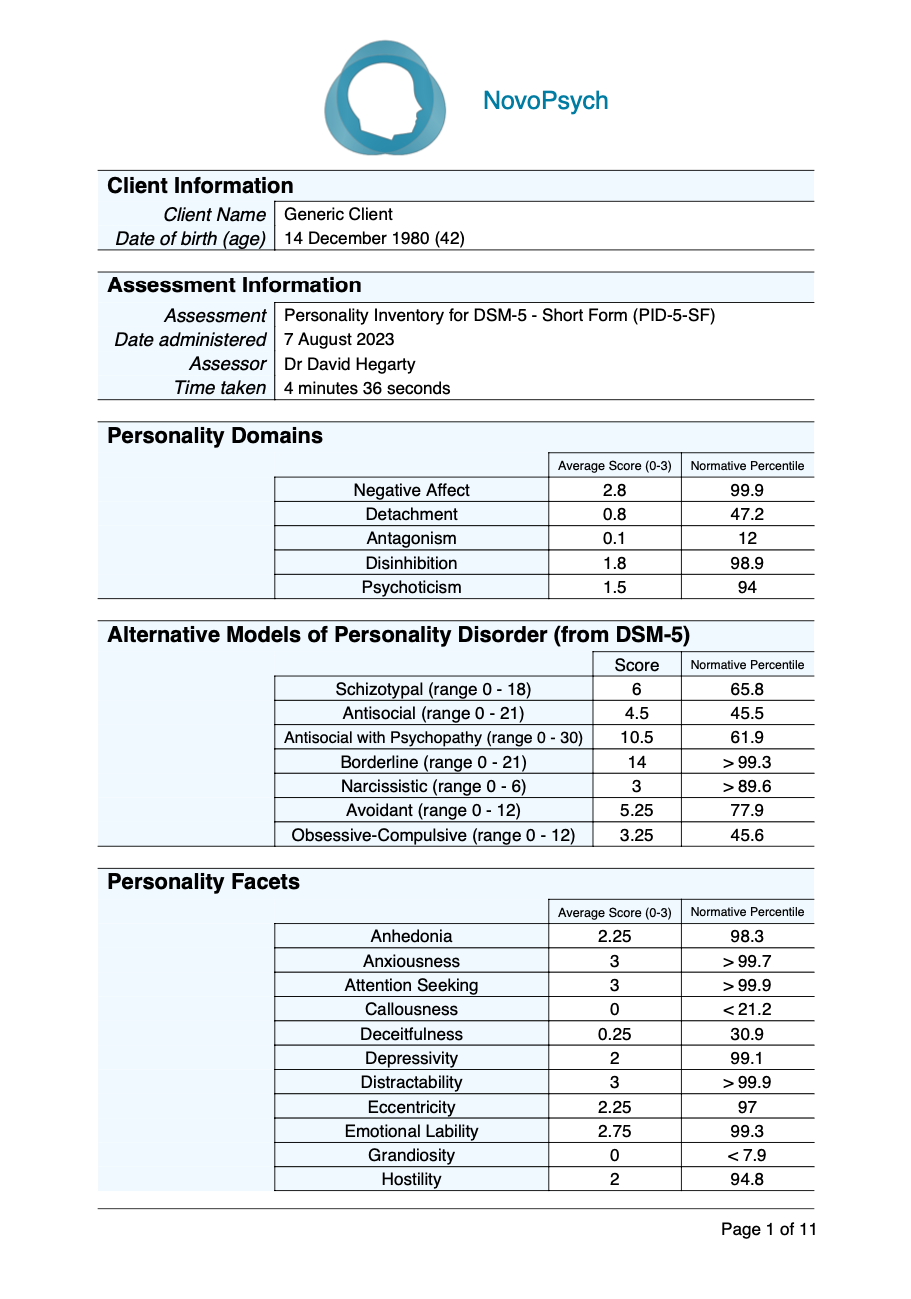
Normative data for the BEDSY is from a sample of 2,663 school students (Spence & Rapee, 2022):
Males
- 11-13 y.o. (M = 4.23, SD = 3.81)
- 14-17 y.o. (M = 3.85, SD = 3.92)
- Combined (M = 4.06, SD = 3.87)
Females
- 11-13 y.o. (M = 5.00, SD = 4.42)
- 14-17 y.o. (M = 6.21, SD = 4.99)
- Combined (M = 5.53, SD = 4.72)
Males and Females Combined
- 11-13 y.o. (M = 4.63, SD = 4.15)
- 14-17 y.o. (M = 5.05, 4.65)
- Combined (M = 4.81, SD = 4.38)
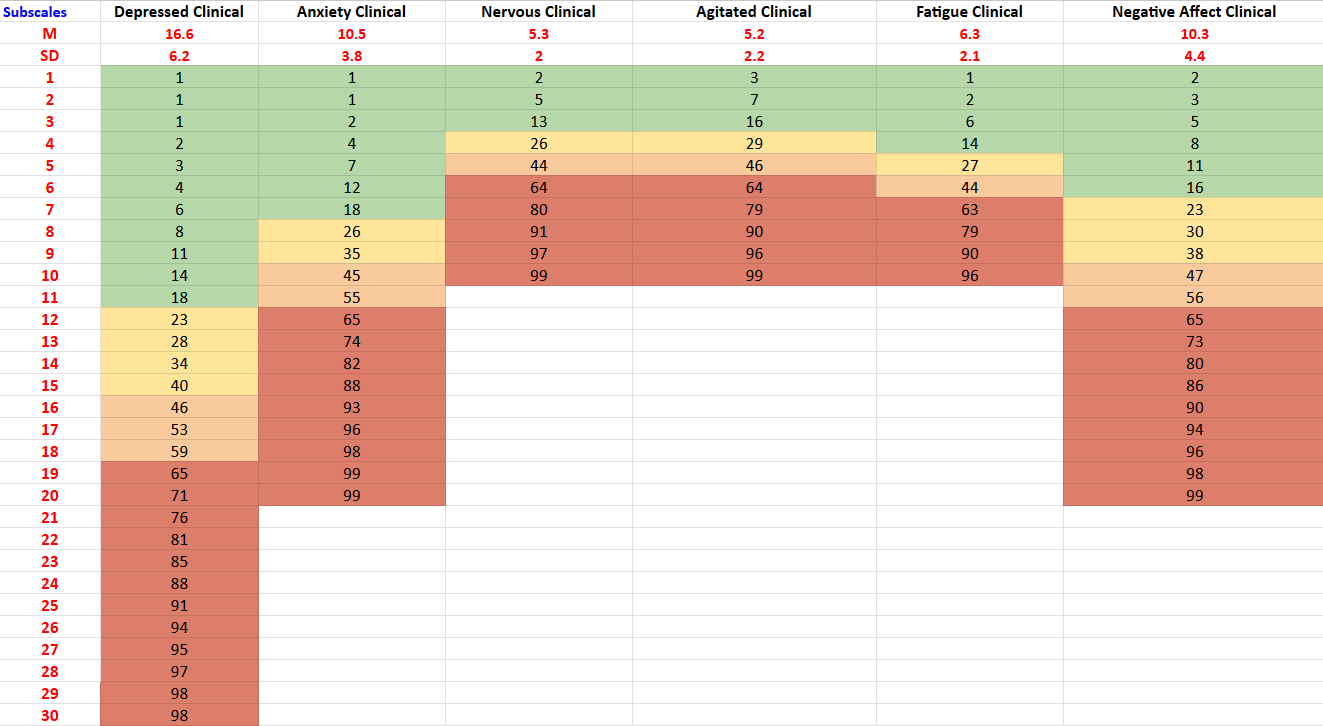
Male and female percentiles are calculated from percentile tables (S. H. Spence & R. M. Rapee, personal communication, May 1, 2024). The male percentile table is for 11-17 year olds as there was no difference between the results for different age groups, however the female percentile table is split up by age group. If no gender or non-binary gender is indicated for the client or if the client is outside the recommended age group for the BEDSY (11-17), then the means and standard deviations above are used to calculate percentiles using an appropriate comparison group (e.g., combined gender, combined age-group).
The scores are categorised into five severity ranges based upon percentiles:
- Normal: Percentile of less than 84
- Mild: Percentile of 84 or greater and less than 94
- Moderate: Percentile of 94 or greater and less than 98
- Severe: Percentile of 98 or greater
Given percentiles are age and gender specific, there are different cut points for severity categories for each group. For example, males score in the Severe range with a score of 14 or above, while females aged between 11-13 require a score of 17 or above, and females 14-17 require a score of 19. These different cut points are designed to respond to different levels of normative patterns of responding for each group.
Changes scores on the BEDSY are based upon the Minimally Important Difference (MID; Norman, Sloan & Wyrwich, 2003) between the initial score and the latest administration. The threshold score for the MID is defined as a half standard deviation (based upon the normative data available) and rounded to the nearest whole number. The MID change score is 2 points or more on the BEDSY total score.
For more information about the BEDSY, see the BEDSY website.
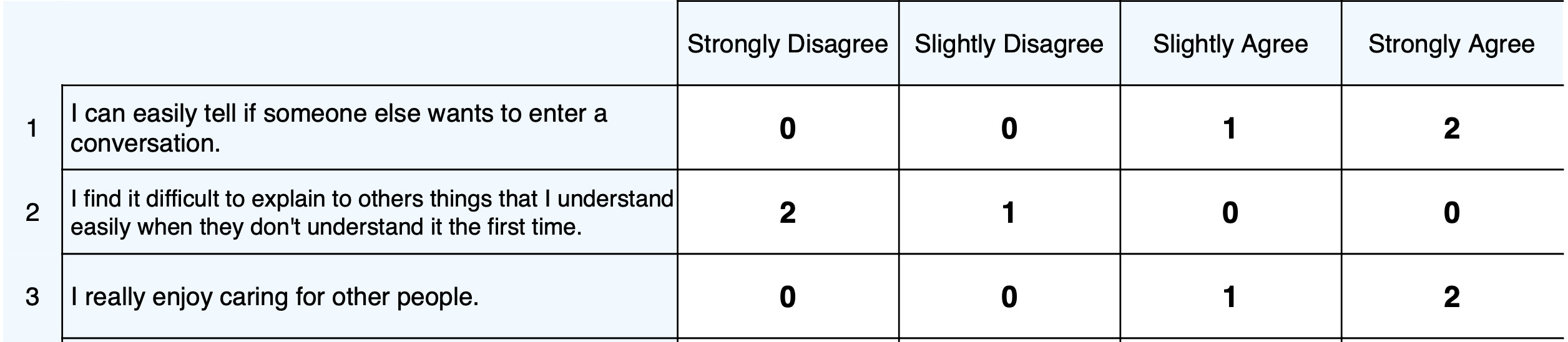
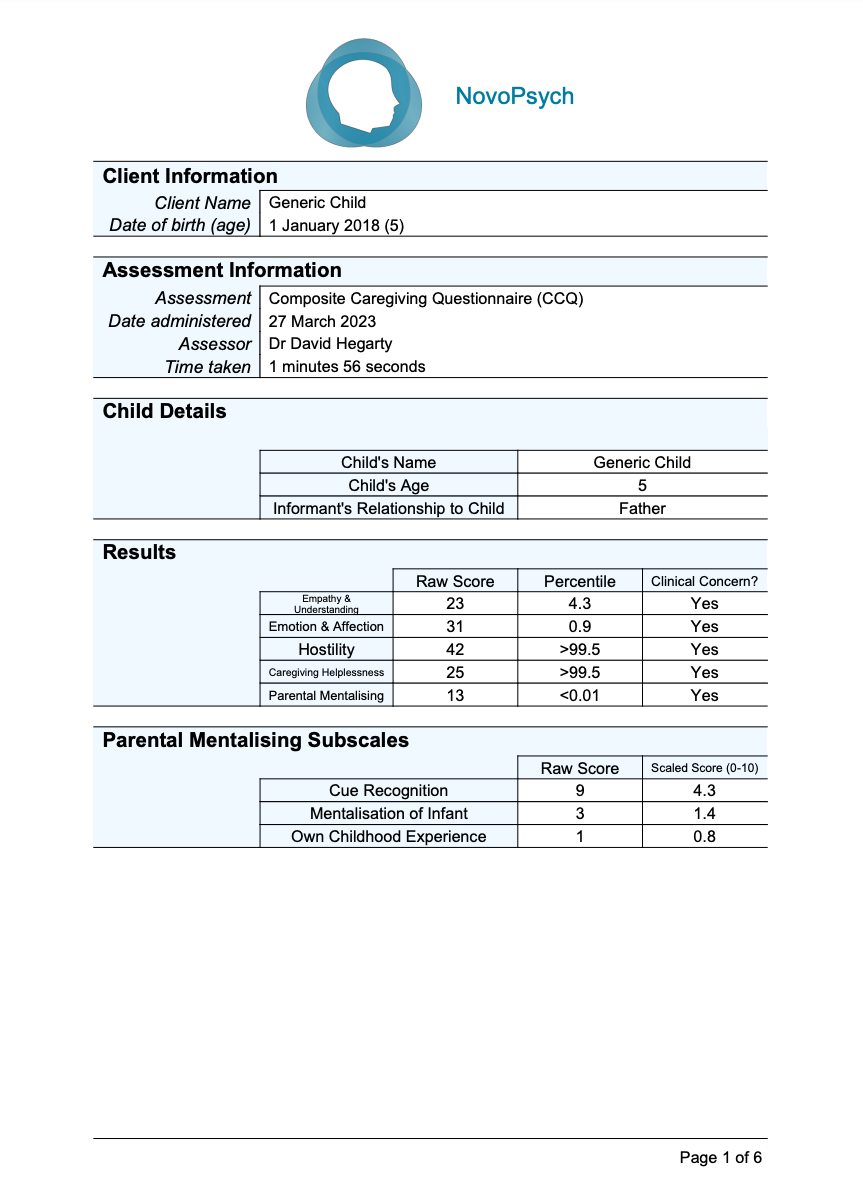
Supplementary Material
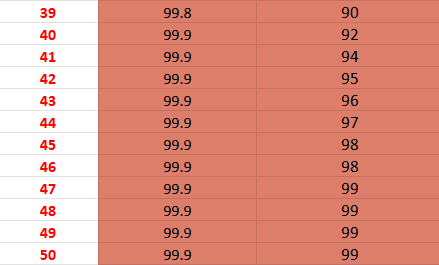
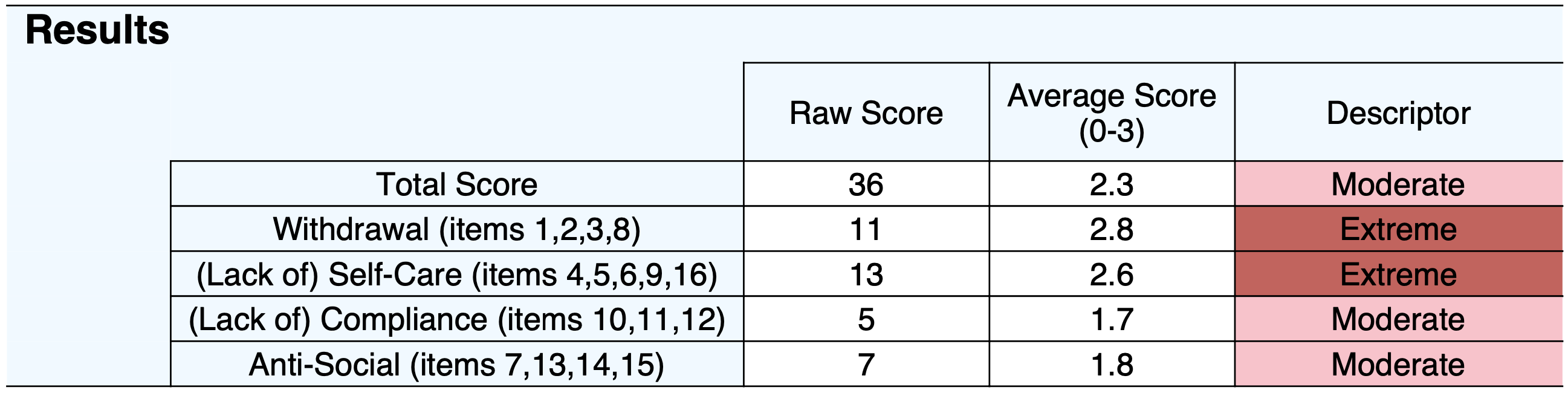
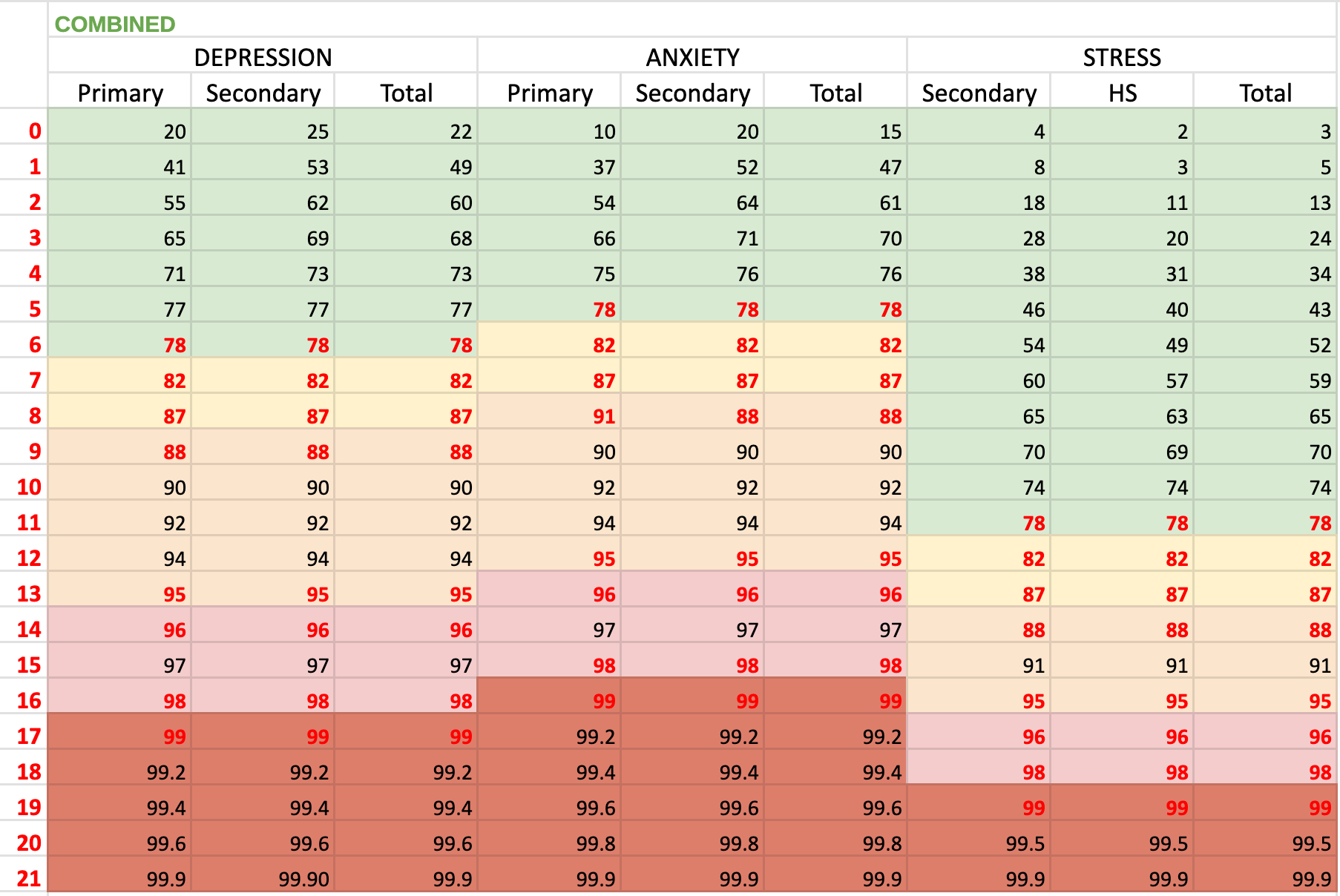
The table below illustrates the gender and age-specific (for females and combined only) normative data (S. H. Spence & R. M. Rapee, personal communication, May 1, 2024). NovoPsych uses this table to calculate percentiles for each score and are based upon male, female or combined and also age for females and combined. For example, to calculate a percentile for a female who is 12 years-old who scored 6 on the BEDSY, we can see that (in the Females 11-13 column) a score of 6 corresponds to a percentile of 73. The colours in the background of the percentiles match the descriptors (Normal = green; Mild = yellow; Moderate = orange; Severe = red).
Developer
Spence, S. H., & Rapee, R. M. (2022). The development and preliminary validation of a brief scale of emotional distress in young people using combined classical test theory and item response theory approaches: The Brief Emotional Distress Scale for Youth (BEDSY). Journal of Anxiety Disorders, 85, 102495–102495. https://doi.org/10.1016/j.janxdis.2021.102495
References
Norman, G. R., Sloan, J. A., & Wyrwich, K. W. (2003). Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Medical care, 41(5), 582–592. https://doi.org/10.1097/01.MLR.0000062554.74615.4C
Spence, S. H., & Rapee, R. M. (2022). The development and preliminary validation of a brief scale of emotional distress in young people using combined classical test theory and item response theory approaches: The Brief Emotional Distress Scale for Youth (BEDSY). Journal of Anxiety Disorders, 85, 102495–102495. https://doi.org/10.1016/j.janxdis.2021.102495




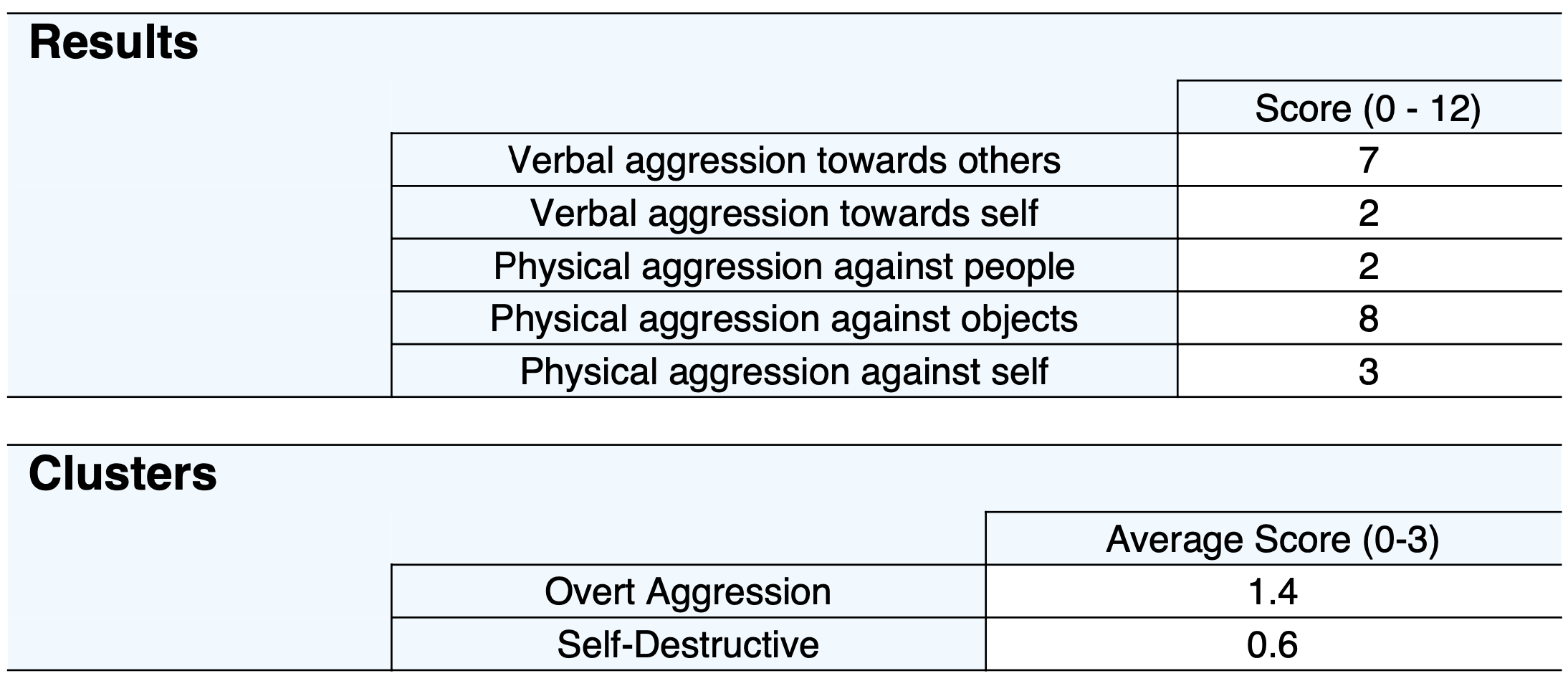














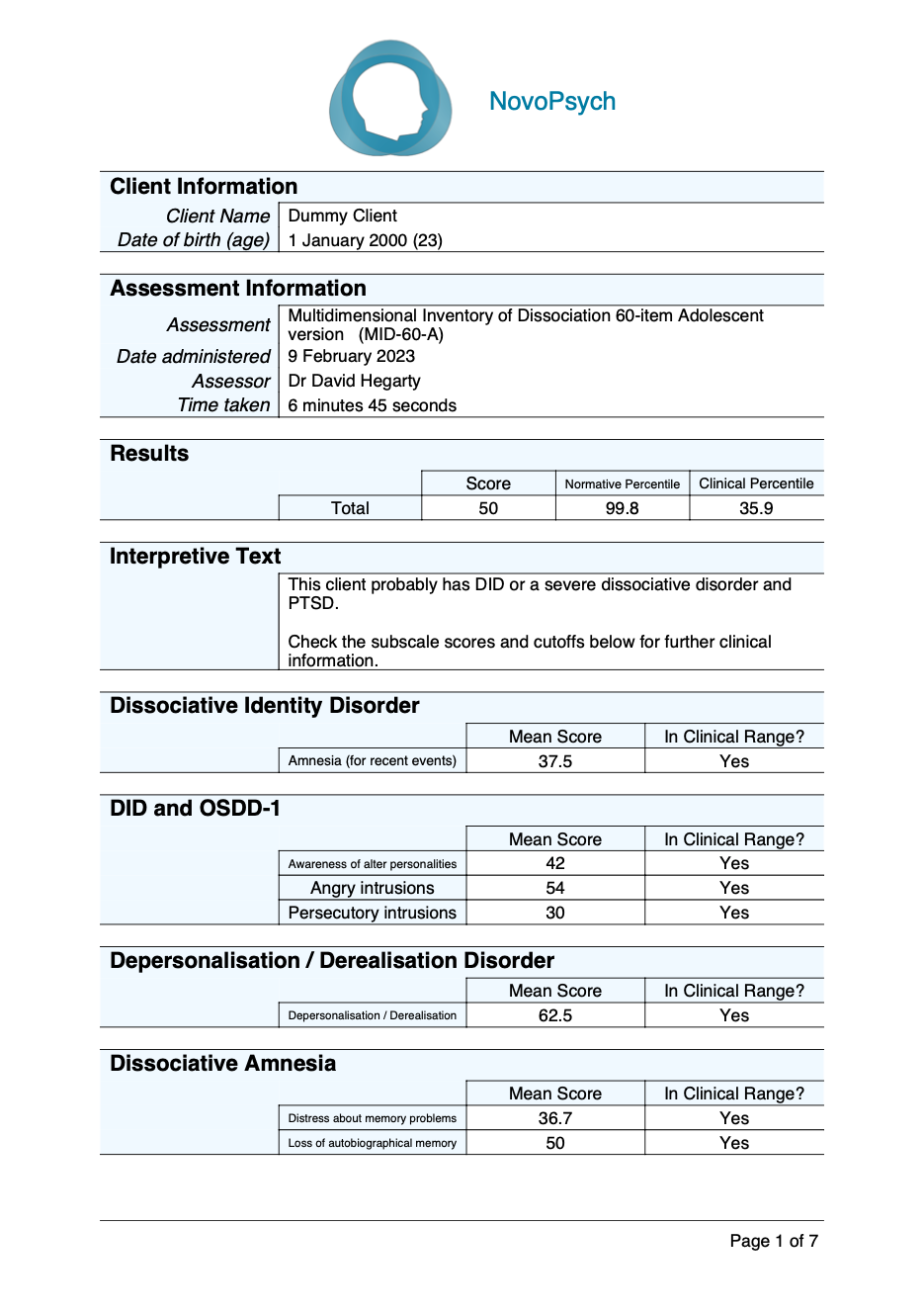





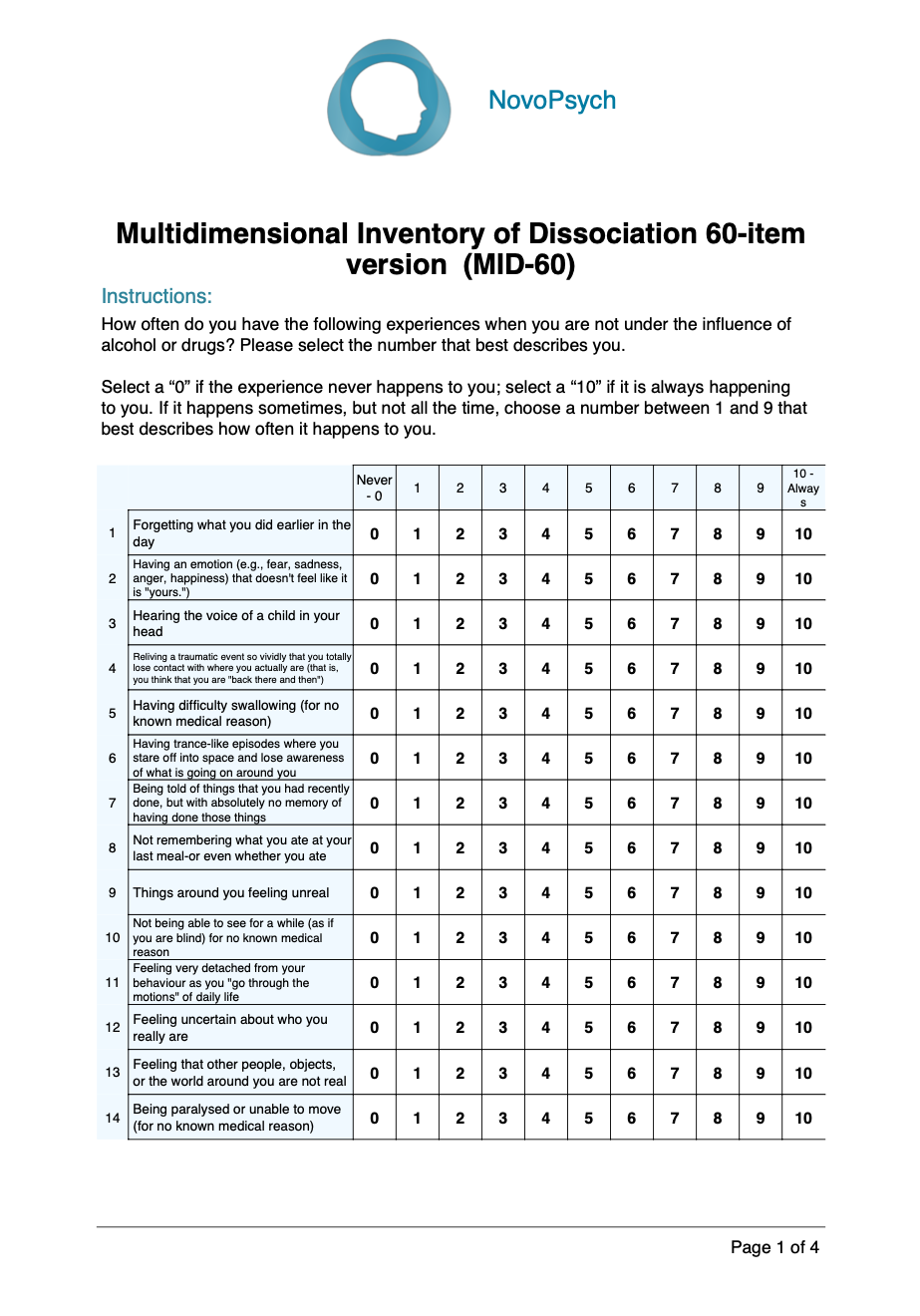
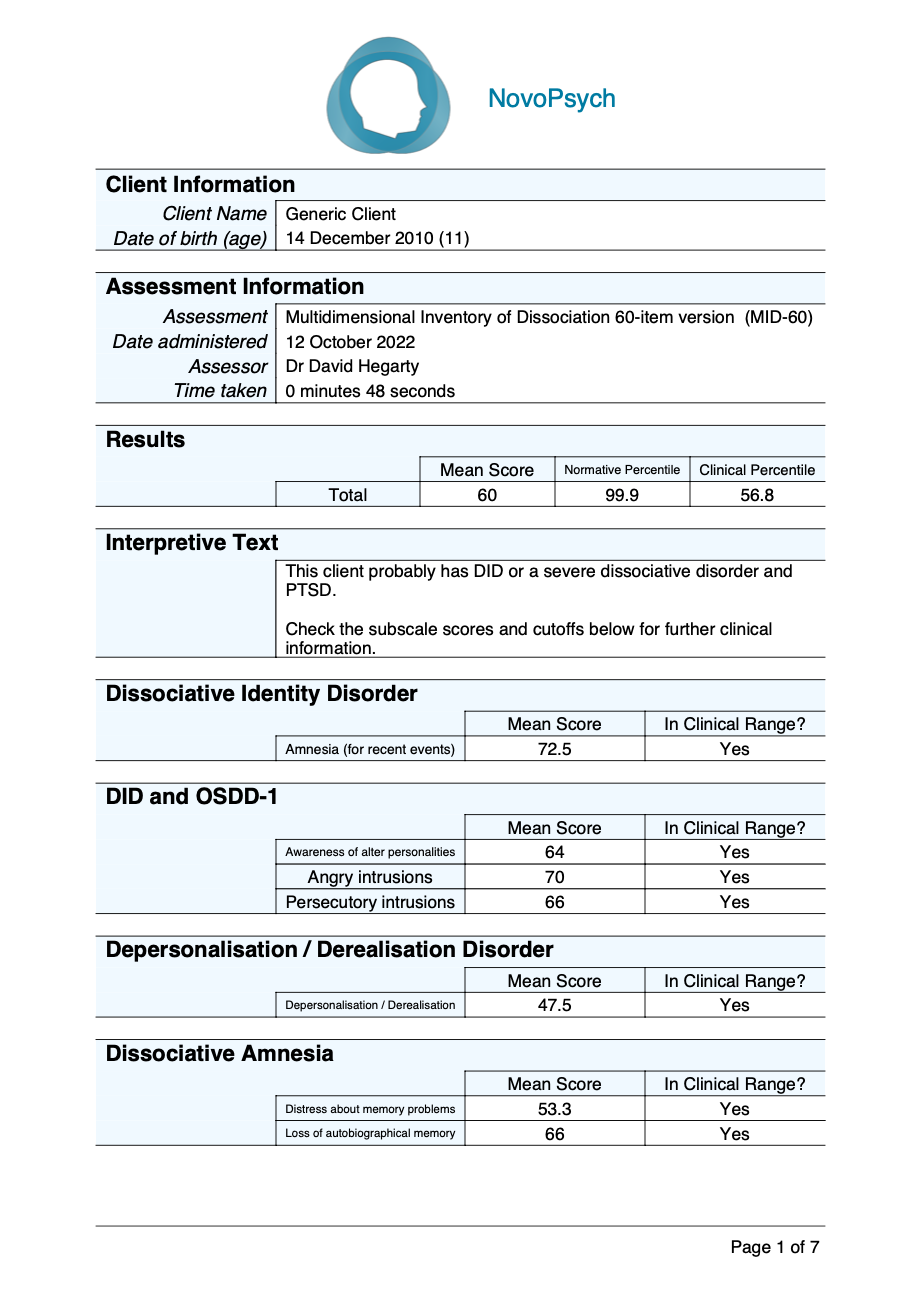
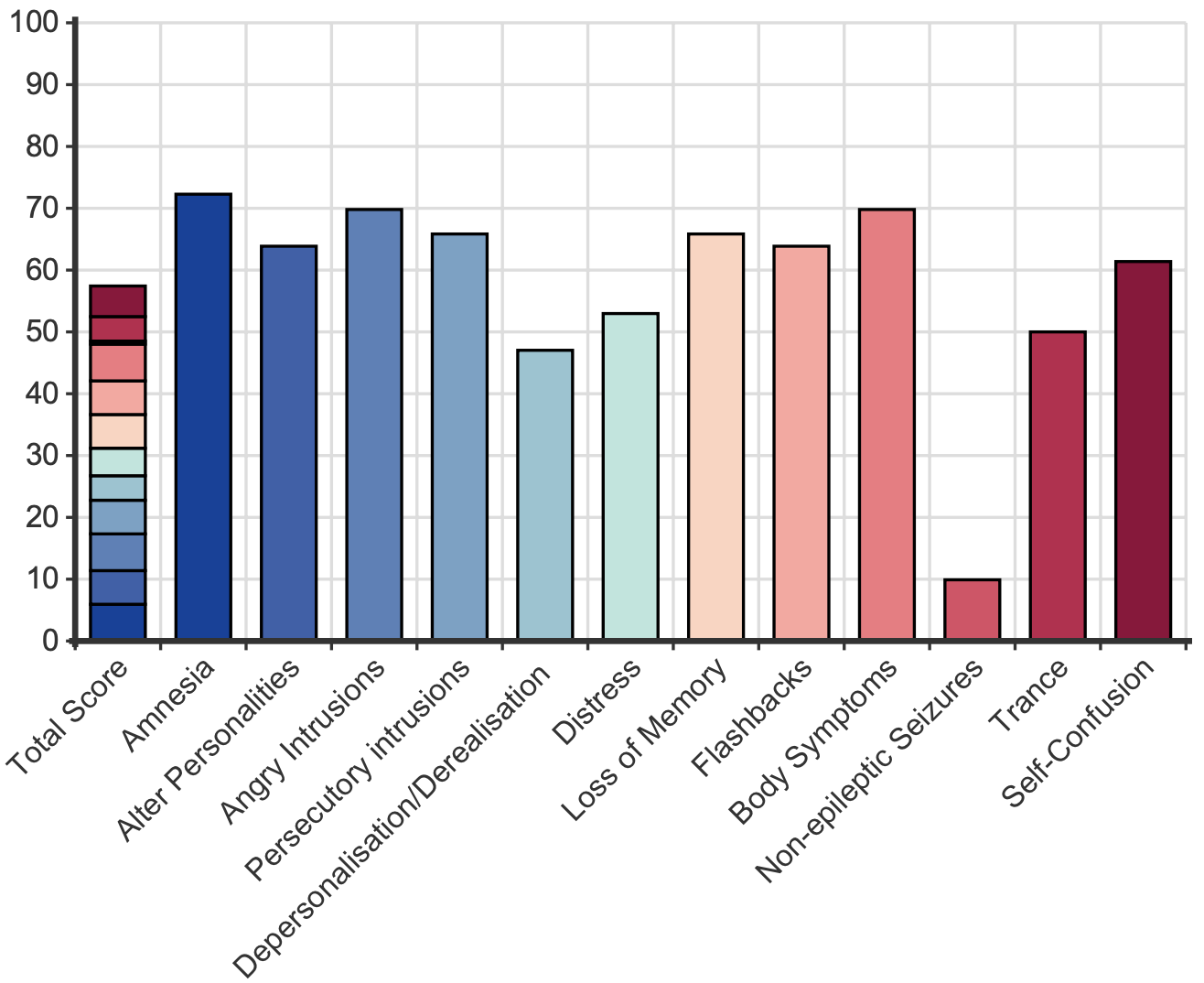 Scores for each item range from zero (never) to 10 (always). The MID-60 mean score represents the percentage of time the person self-reports having dissociative symptoms and experiences. Hence, a person with dissociative identity disorder may have dissociative symptoms and experiences around half the time (51%) whereas for a university student this may be 13% of the time. A mean score of more than 21% indicates clinically significant symptoms.
Scores for each item range from zero (never) to 10 (always). The MID-60 mean score represents the percentage of time the person self-reports having dissociative symptoms and experiences. Hence, a person with dissociative identity disorder may have dissociative symptoms and experiences around half the time (51%) whereas for a university student this may be 13% of the time. A mean score of more than 21% indicates clinically significant symptoms.