The highly successful program for Medicare subsided sessions with psychologists has had two major shortcomings:
1. – The fact the 10 sessions is not enough for many patients
2. – The limited evaluation of the effectiveness of these MBS services.
I’d like to take the time to share my thoughts on the future of Medicare psychology services in Australia, in light of the Productivity Commission’s recommendations.
If mandatory outcome monitoring is to be introduced, as the draft report suggests, I’d propose that psychologists be invited to participate in a program evaluation process that requires collection of outcome data and those who enrol be allowed to provide 20 sessions per calendar. The strategy of linking funding for extra sessions with participation in evaluation has a number of advantages, including creating an incentive for private psychologists to opt into participating in the initial rollout of outcome monitoring while at the same time evaluating the effectiveness of the increased session numbers.
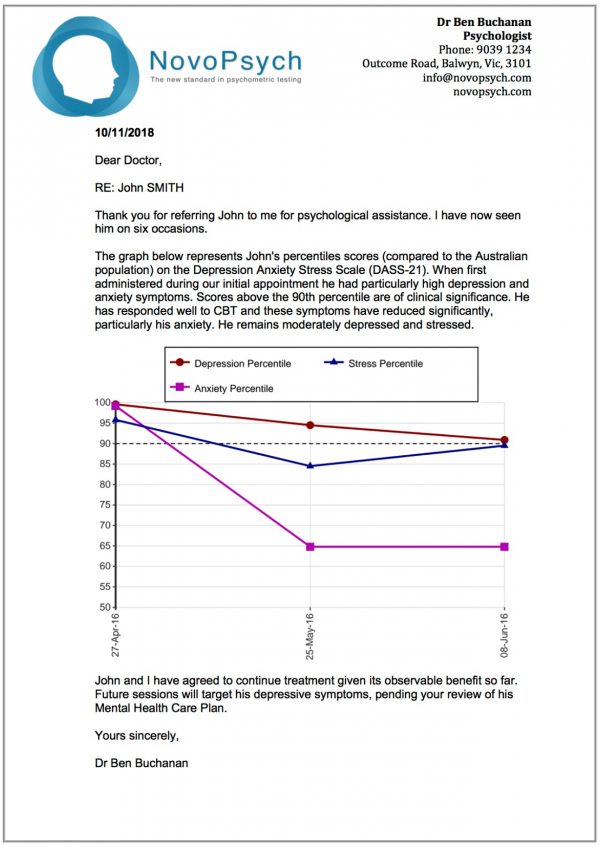
Under the current Better Access model GPs undertake rudimentary and disconnected outcome monitoring, generally by administering a paper copy of the K-10 questionnaire measuring psychological distress. The current process has some serious shortcomings, including that the K-10 data is not systematically transmitted to a central body for evaluation. In addition, outcome monitoring is best done by the treating clinician (e.g. the psychologist) as an intrinsic part of the therapeutic process rather than by a referring party (the GP).
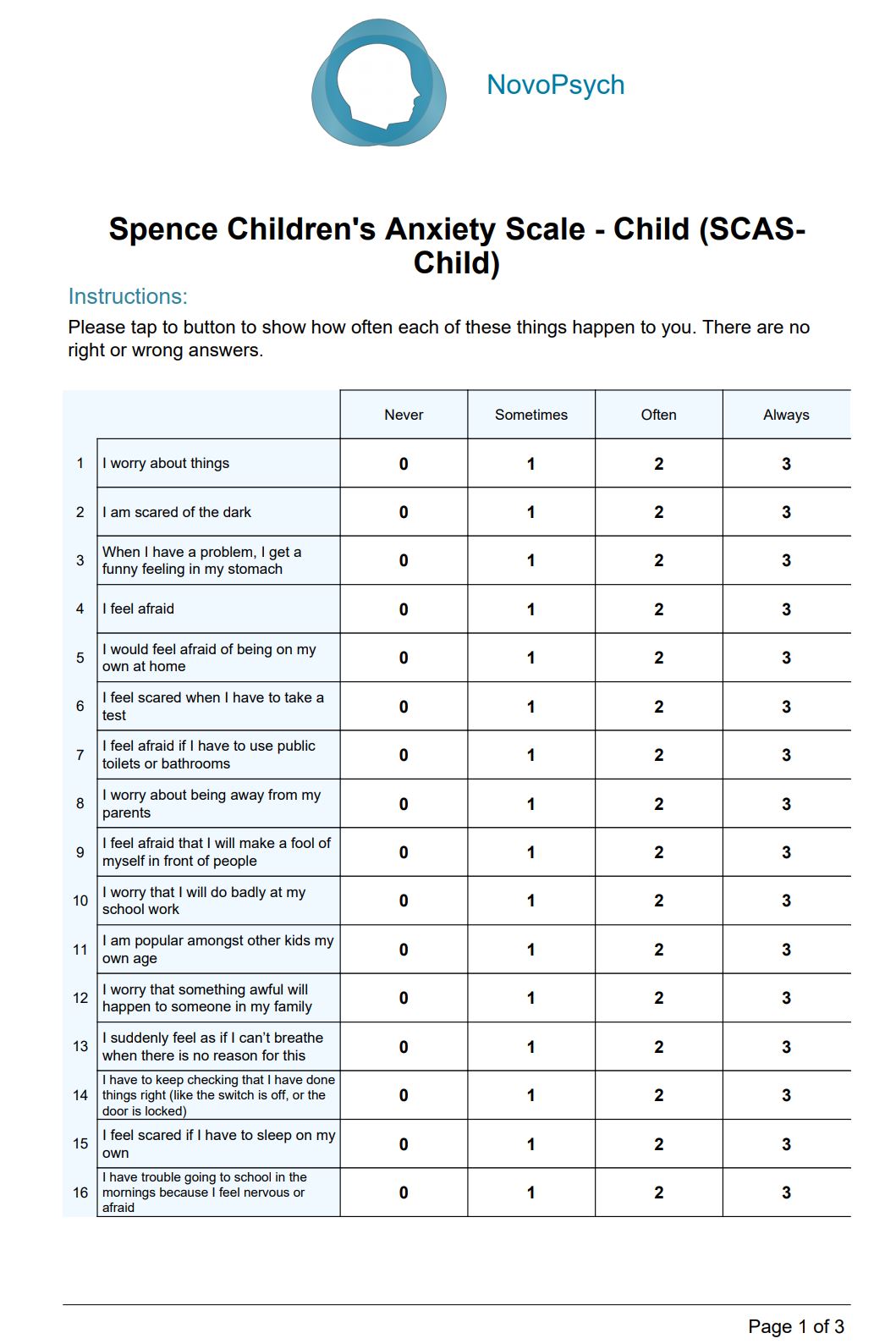
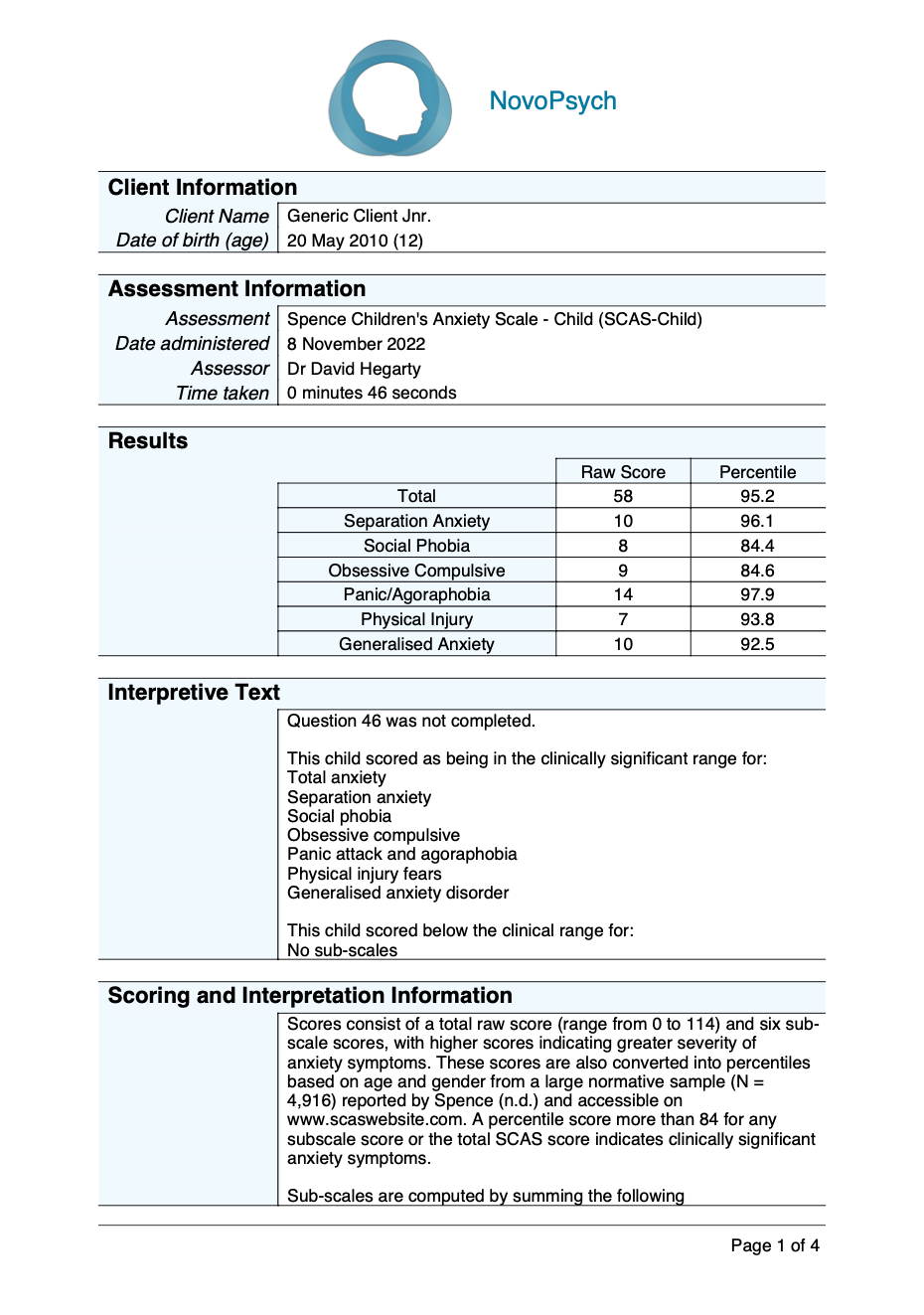
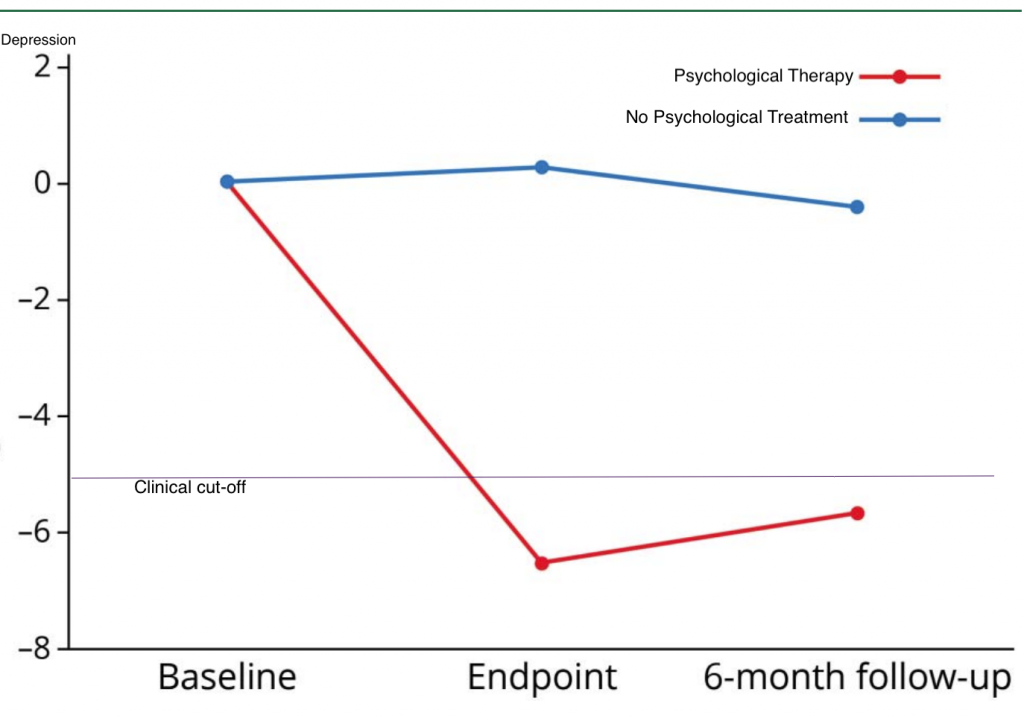
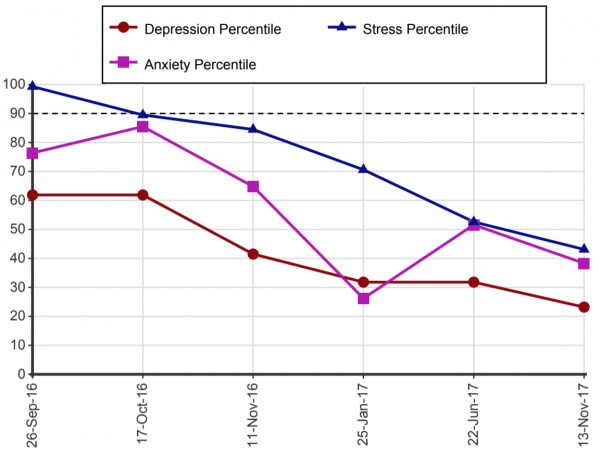
In fact, it is good practice in psychological therapy to administer symptom monitoring scales each session to provide psychologist and client with immediate and objective feedback about their symptoms. A recent paper in Lancet (Delgadillo et al., 2018) found that psychological therapy with continuous symptom monitoring increases the effectiveness of treatment compared to psychological therapy without outcome monitoring and immediate feedback.
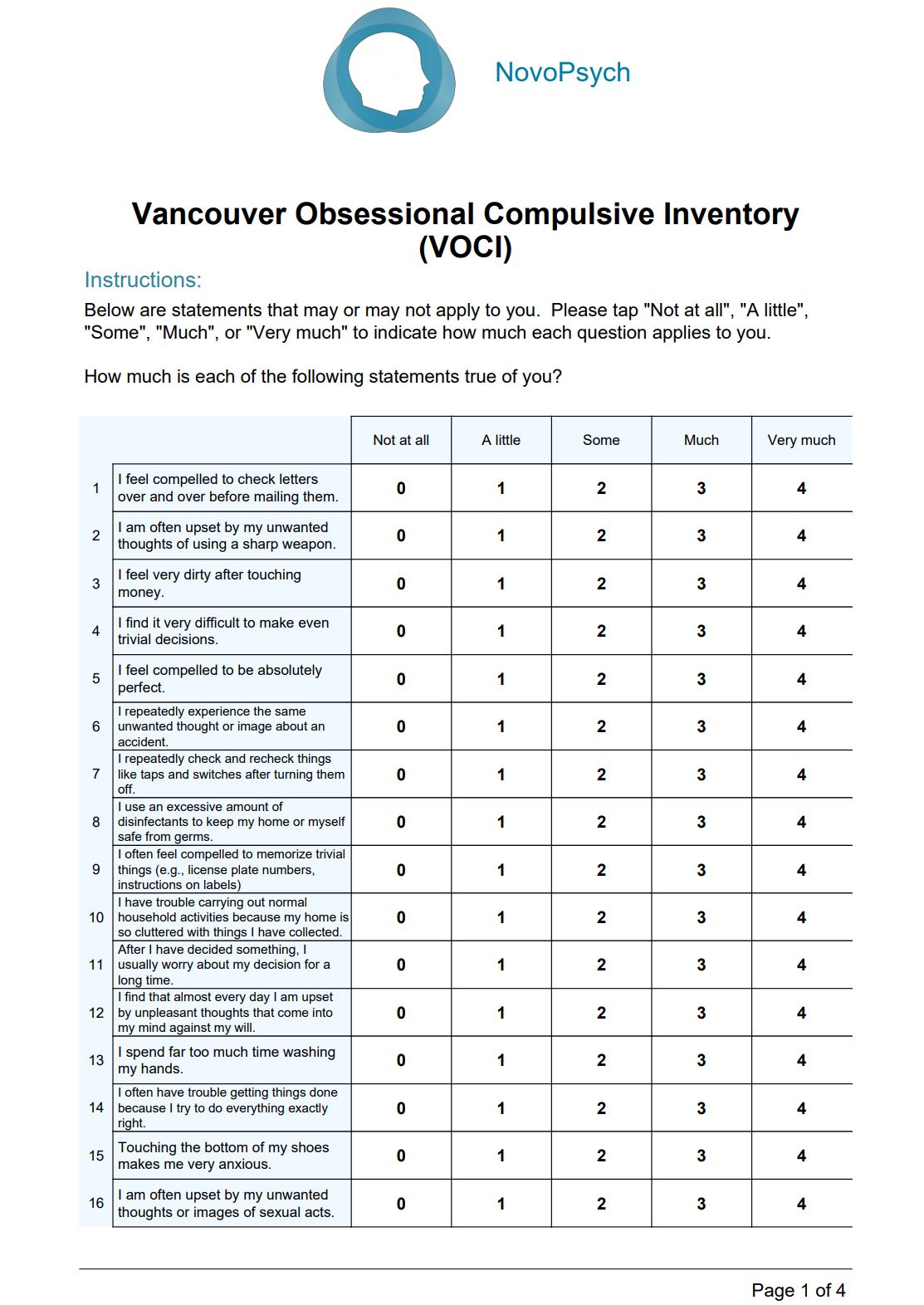
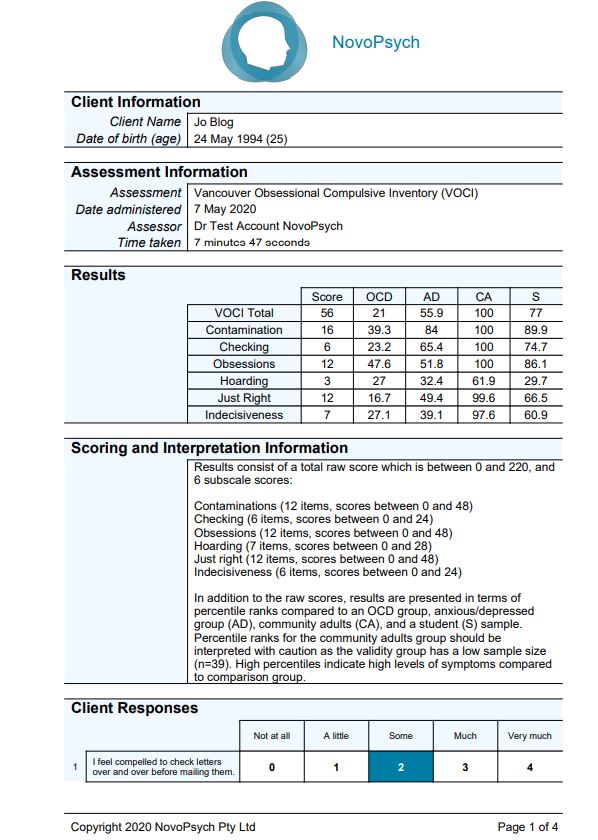
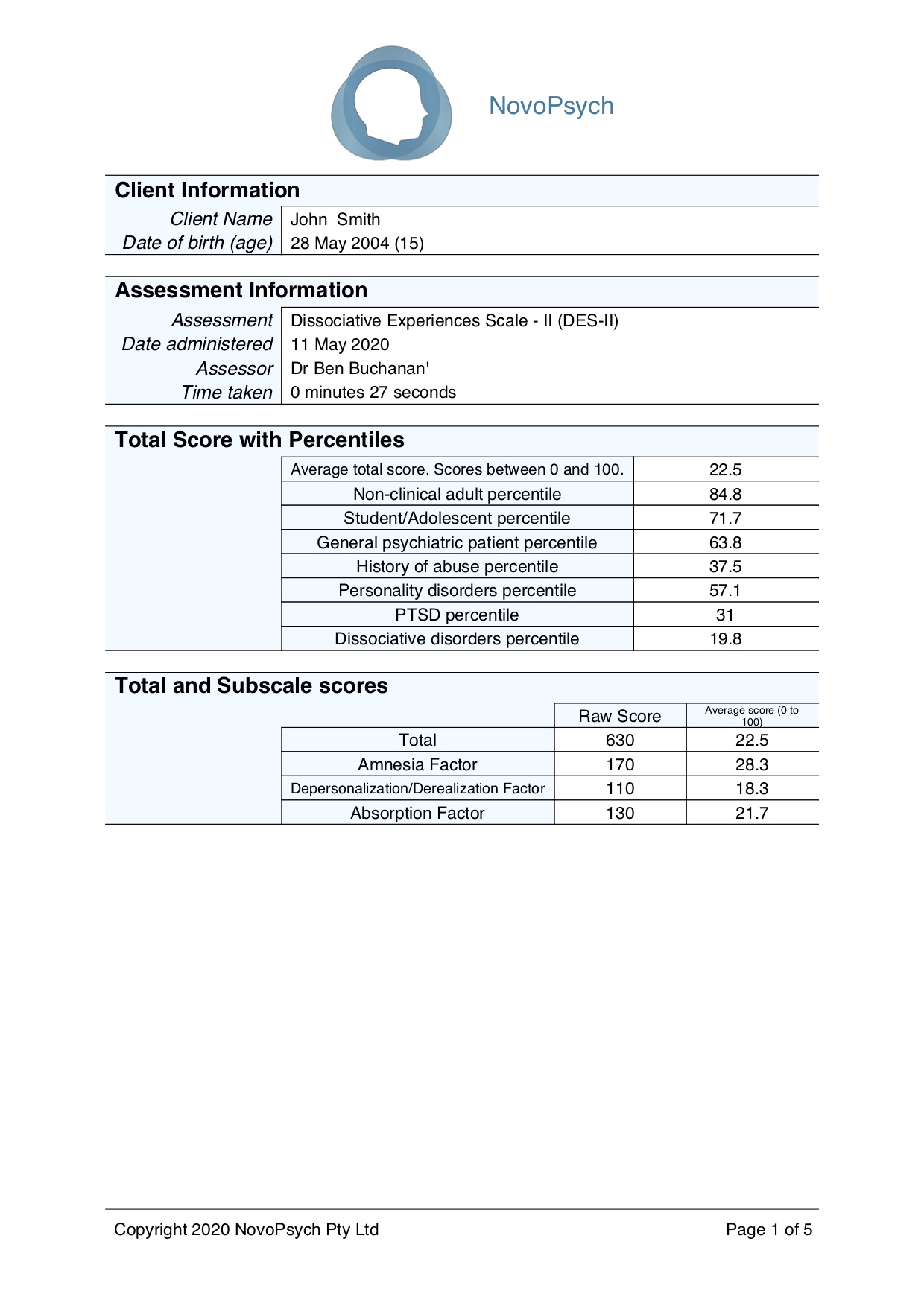
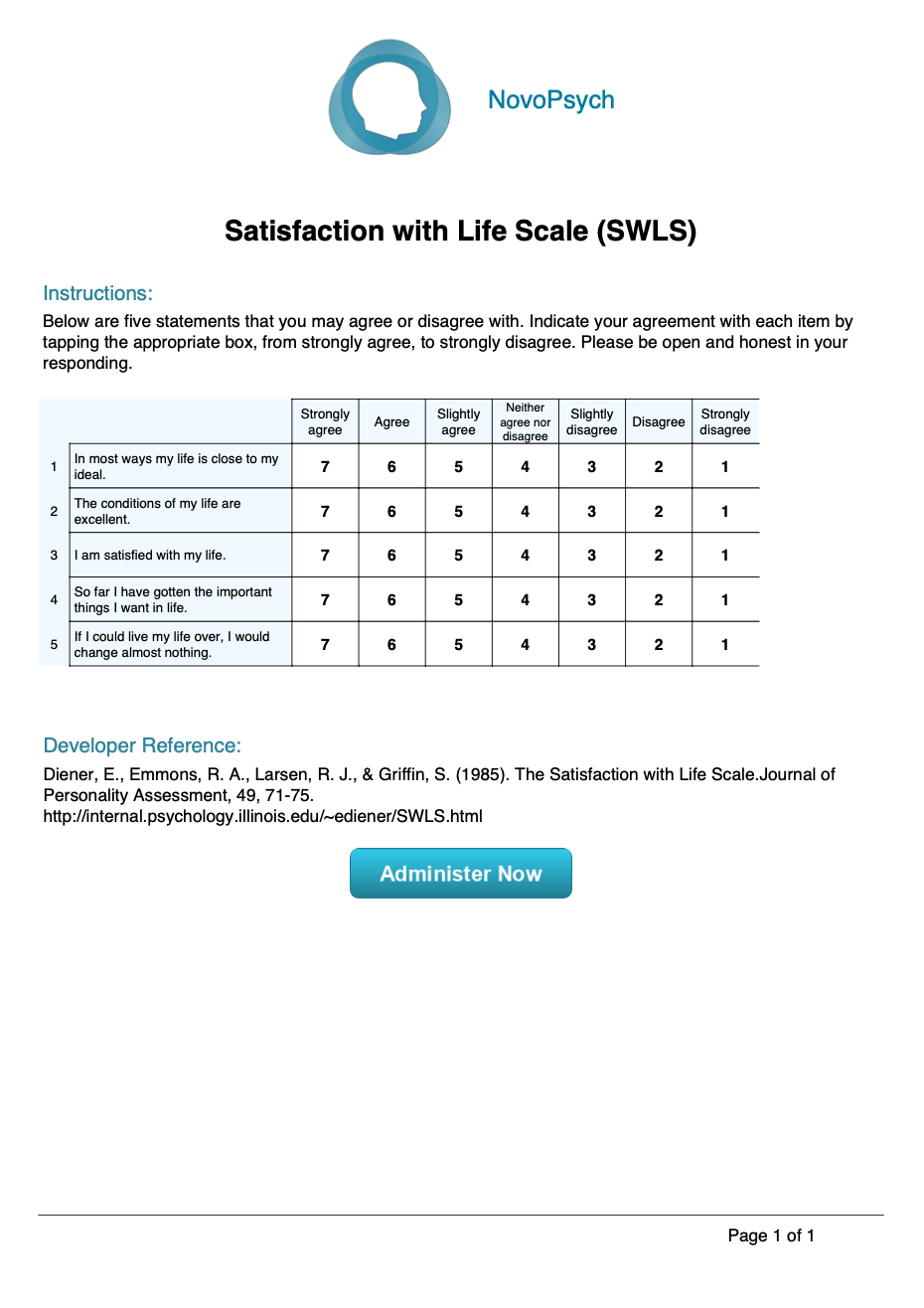
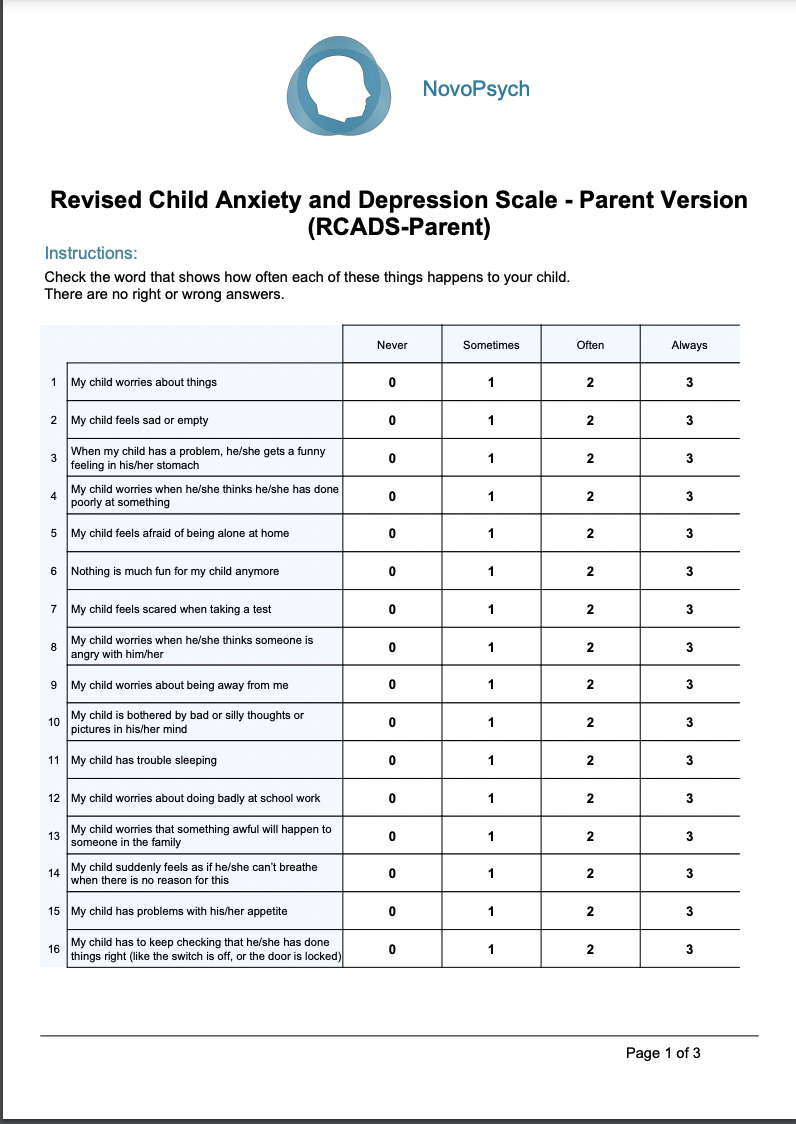
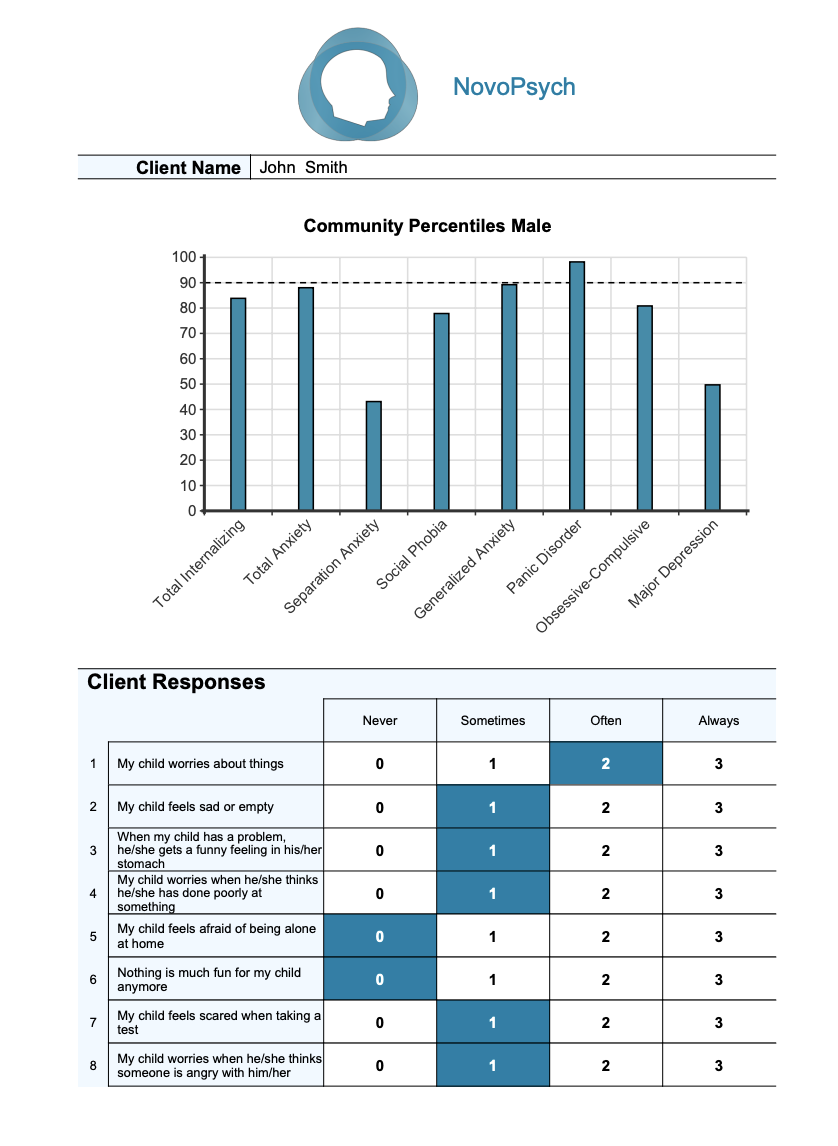
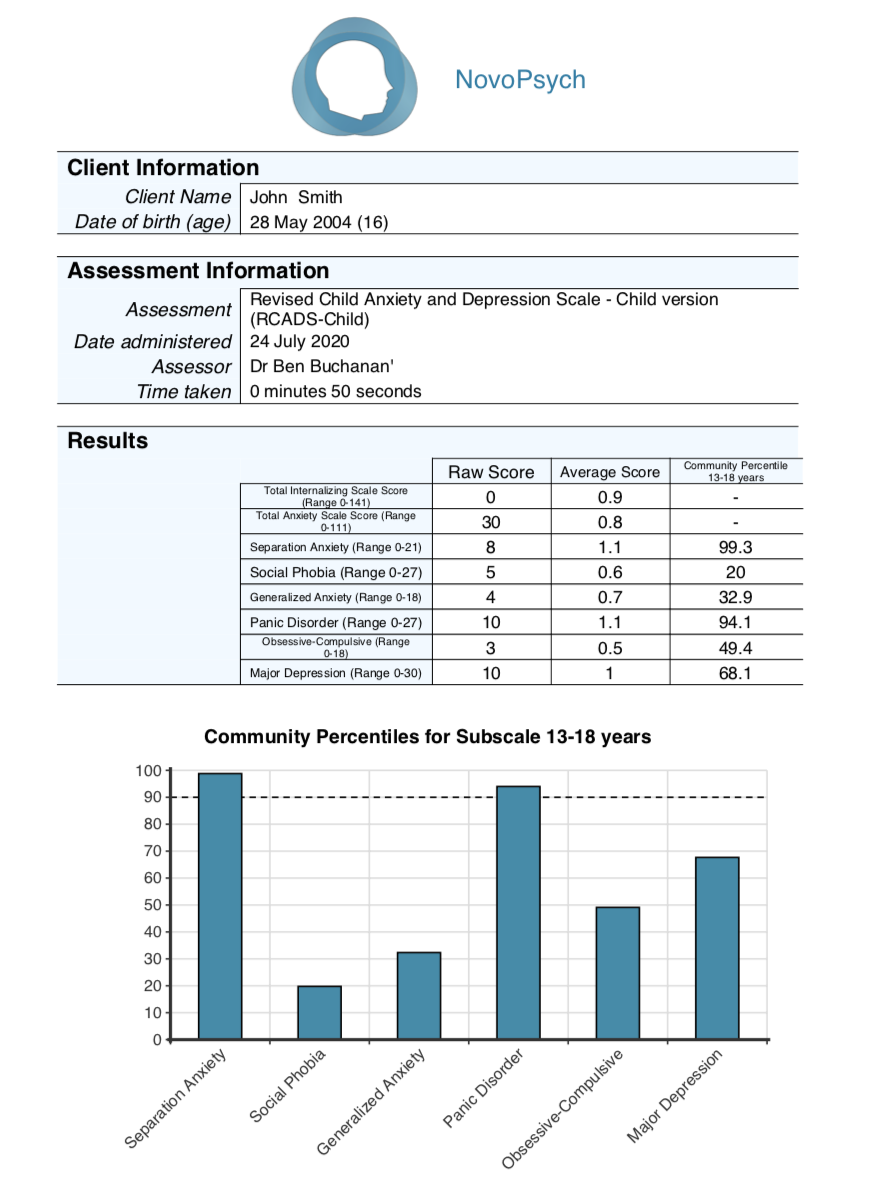
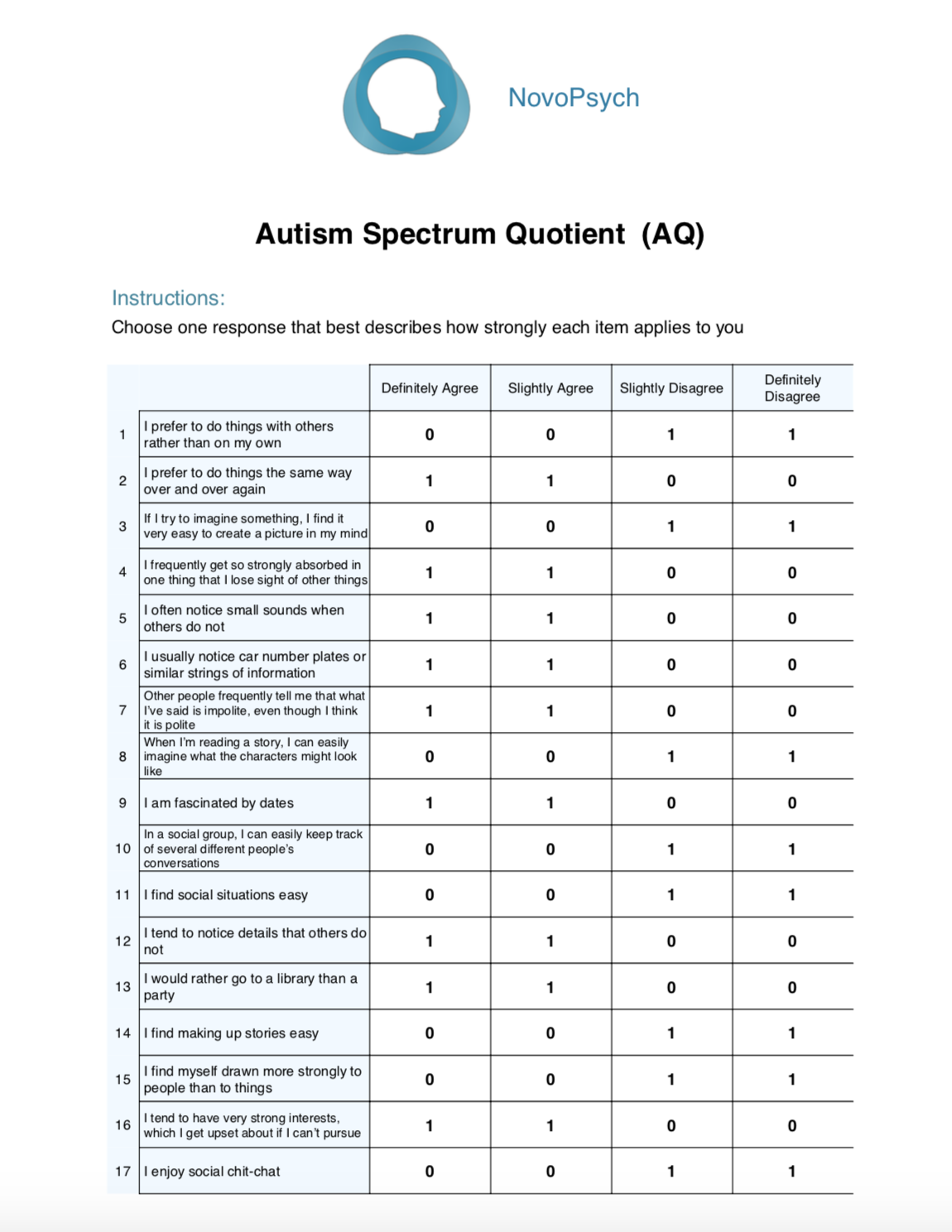
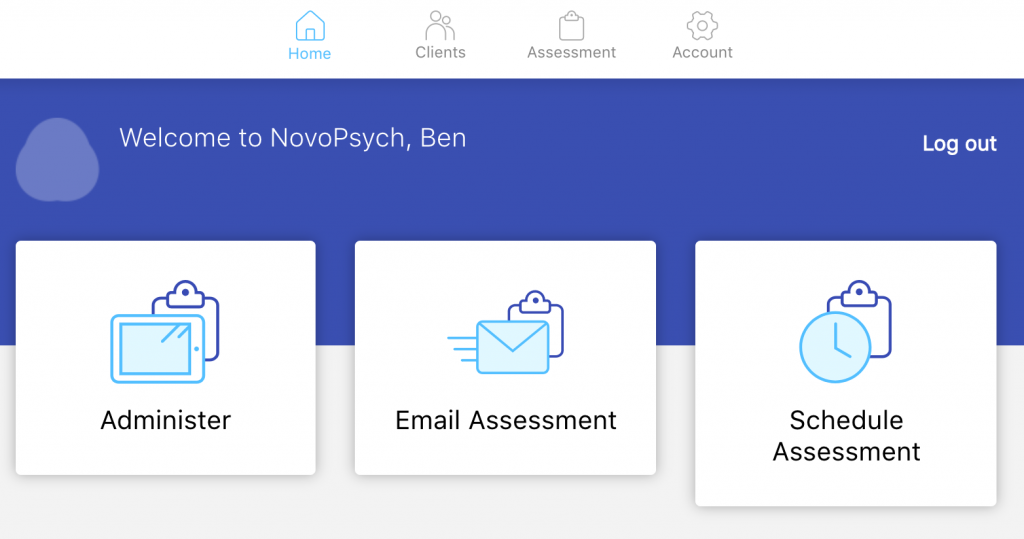
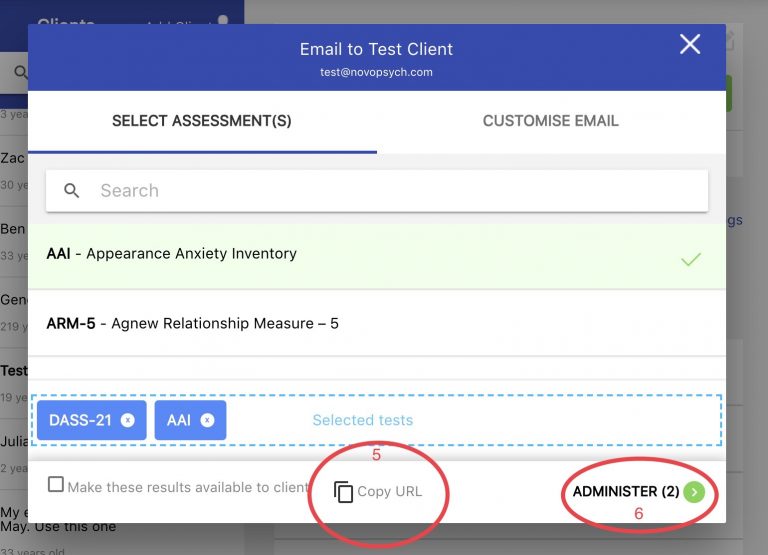
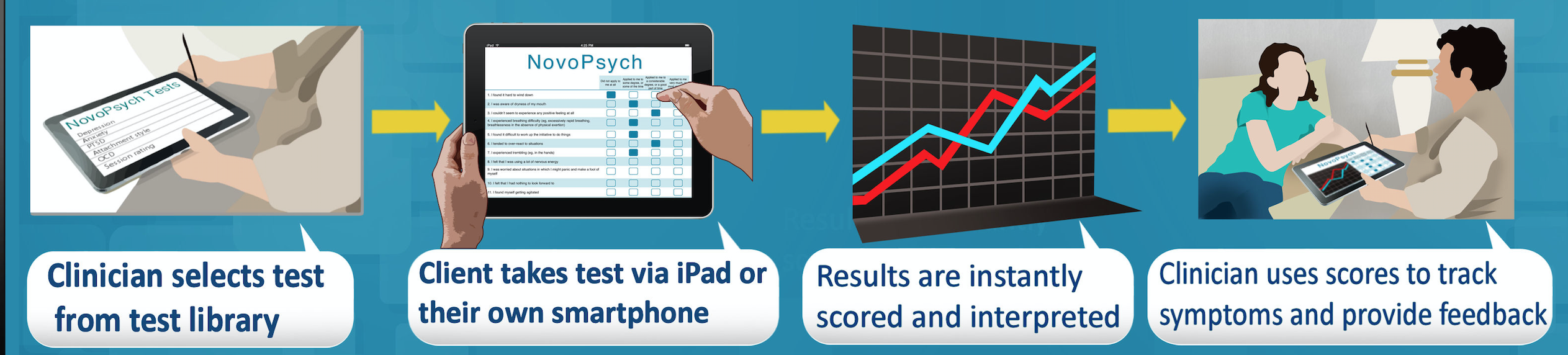
Given the evidence that outcome monitoring within therapy improves outcomes many psychologists are already integrating outcome monitoring into their practice. NovoPsych facilitates this through our software for more than 3000 psychologists.
We suggest that the administration of outcome measures for the proposed trial of 20 sessions of MBS funded psychological therapy be collected by psychologists (rather than the GP). MBS items could be structured such that a requirement be that an outcome measurement tool be administered every psychology session and that the data be digitally transmitted to a central point.
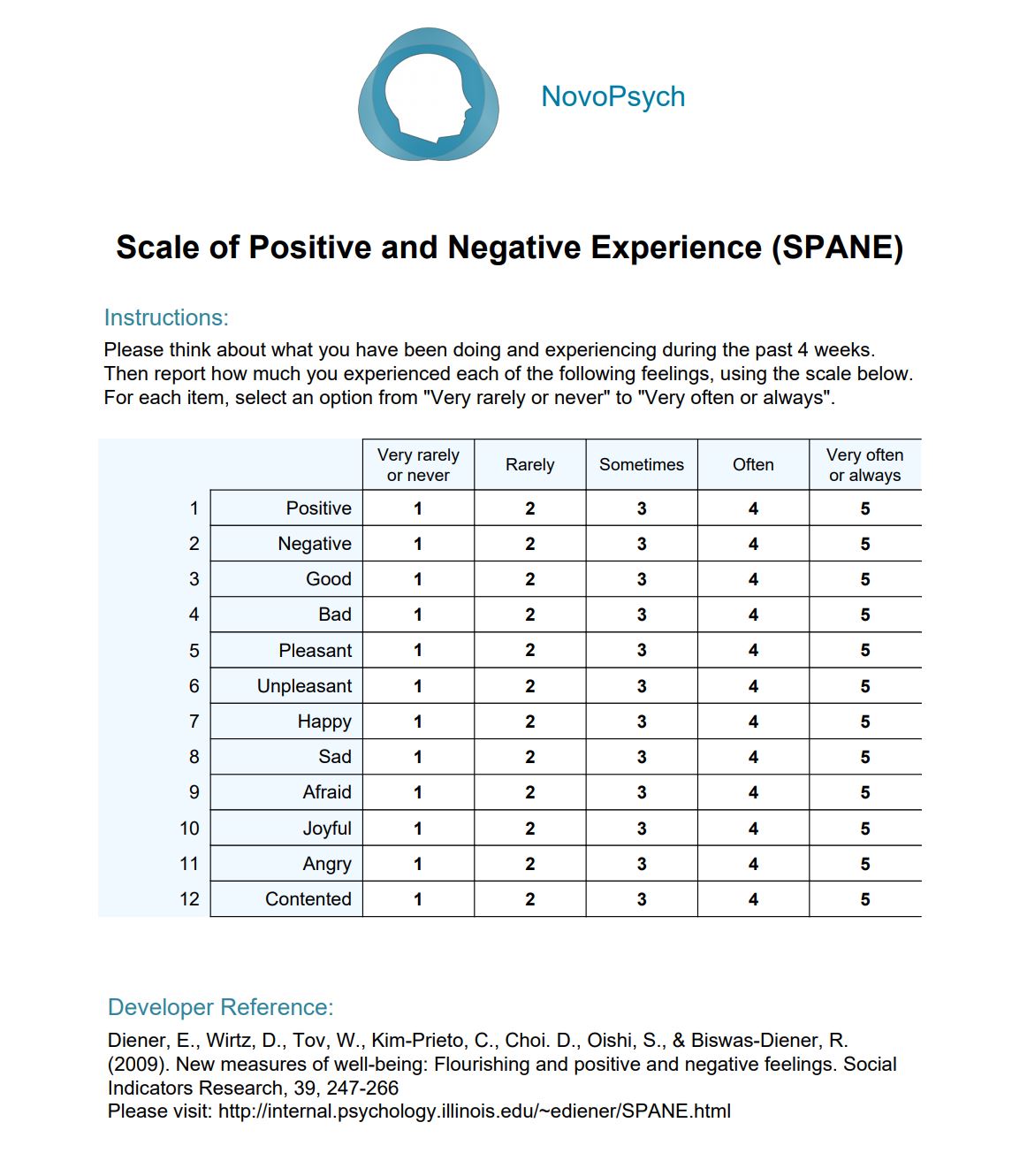
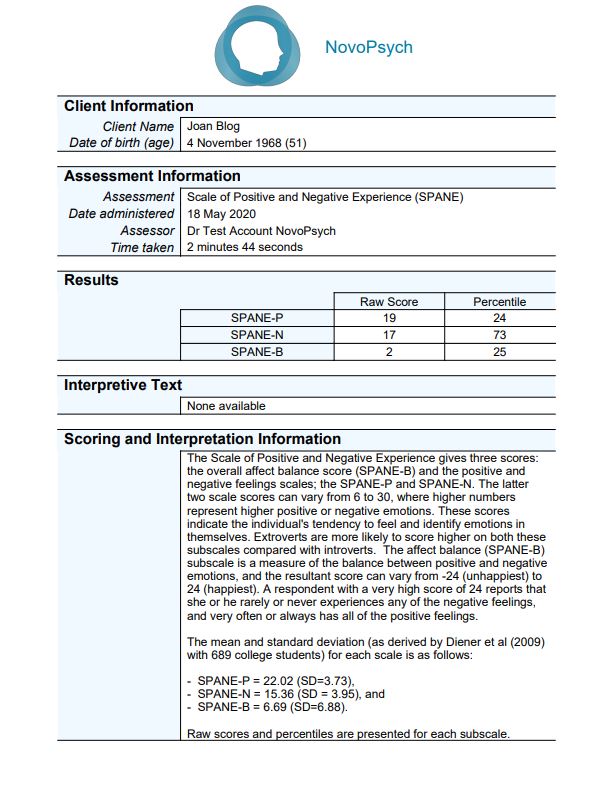
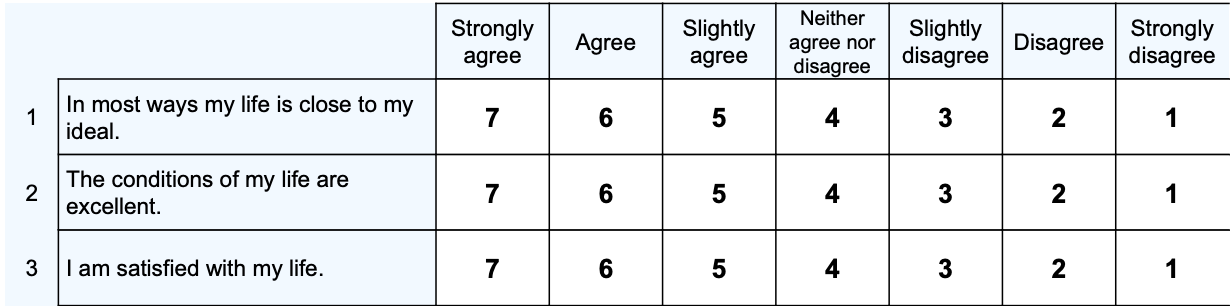
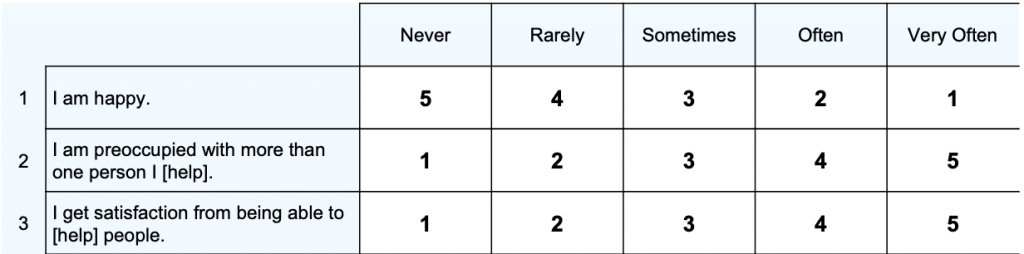
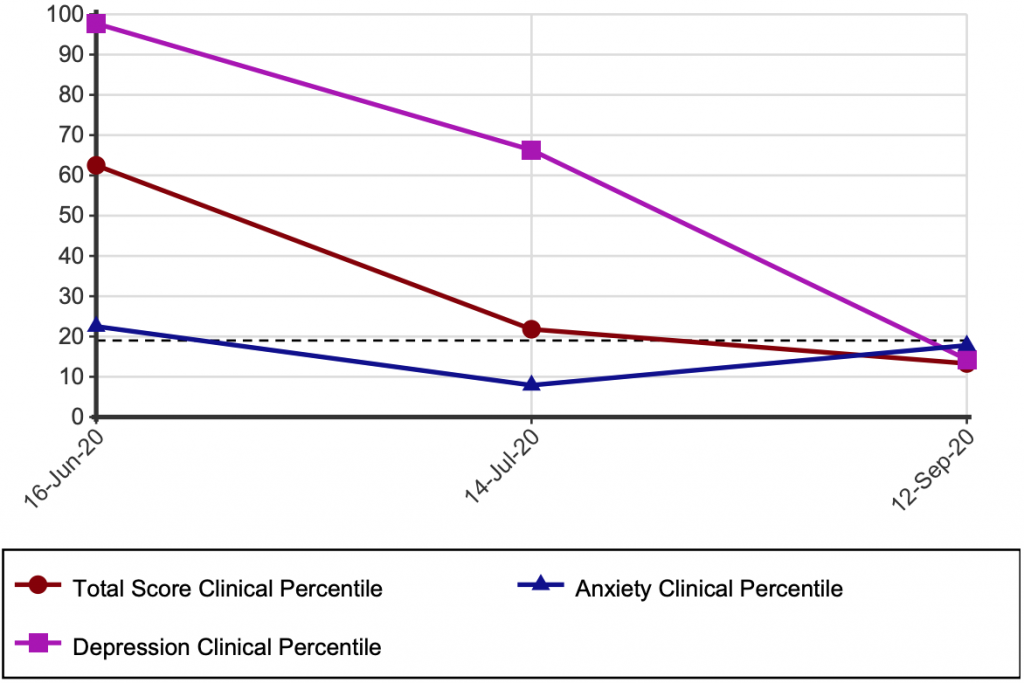
We would suggest the outcome measurement tool be either the Depression Anxiety Stress Scale (DASS-21) or Kessler 10 (K10) given their current wide use and ease of administration. If you’d like our detailed project design please contact Dr Ben Buchanan (details above).
Draft Recommendation 22.5 – Building a Strong Evaluation Culture
A robust culture of program evaluation should inform the allocation of public funds across the mental health system to ensure that they are deployed most efficiently and effectively.
We note that some professions within the mental health workforce have critical training and expertise in program evaluation and outcome measurement, and there is a grass roots effort, particularly among psychologists, to engage in outcome monitoring through the collection of data. Psychology practices that provide sessions subsidised by Medicare could benefit from policy settings that support evaluation culture.
Draft Recommendation 25.3 – Strategies to Fill Data Gaps
Collect the data in a way that imposes the least regulatory burden to ensure data is high-quality and fit-for-purpose– publish the data in ways that are useful to policy makers, service providers and consumers.
It is our experience that practitioners and service providers can be reluctant to collect data given the administrative burden. This is especially true in private practice settings. For example, a survey of Australian Psychologists found the two reasons most often cited for not collecting outcome data was 1) “Takes too long to administer and score” and 2) “Too much of a burden for clients” (Chung & Buchanan 2018).
We’d therefore recommend that the use of outcome monitoring be incentivised by funding models. For example, allowing private psychologists who routinely collect and report outcome data to provide 20 Medicare rebated sessions per year rather than the current 10.
Draft Finding 25.1 Monitoring and Reporting at the Service Provider Level
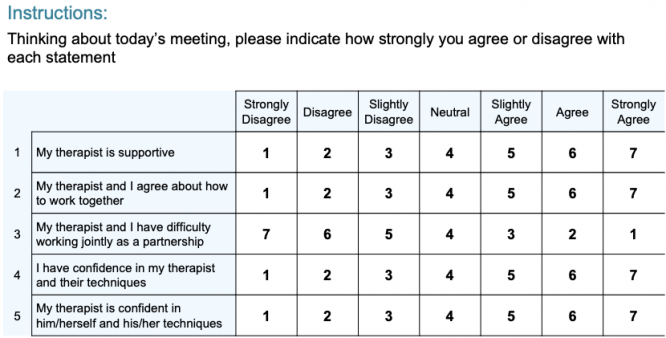
Monitoring and reporting at the provider level can improve transparency and accountability, and potentially service quality, through: · publishing data that informs consumer choice and drives self-improvement · benchmarking analyses, where services are able to regularly compare their performance relative to similar services, that prompt discussions and information sharing.
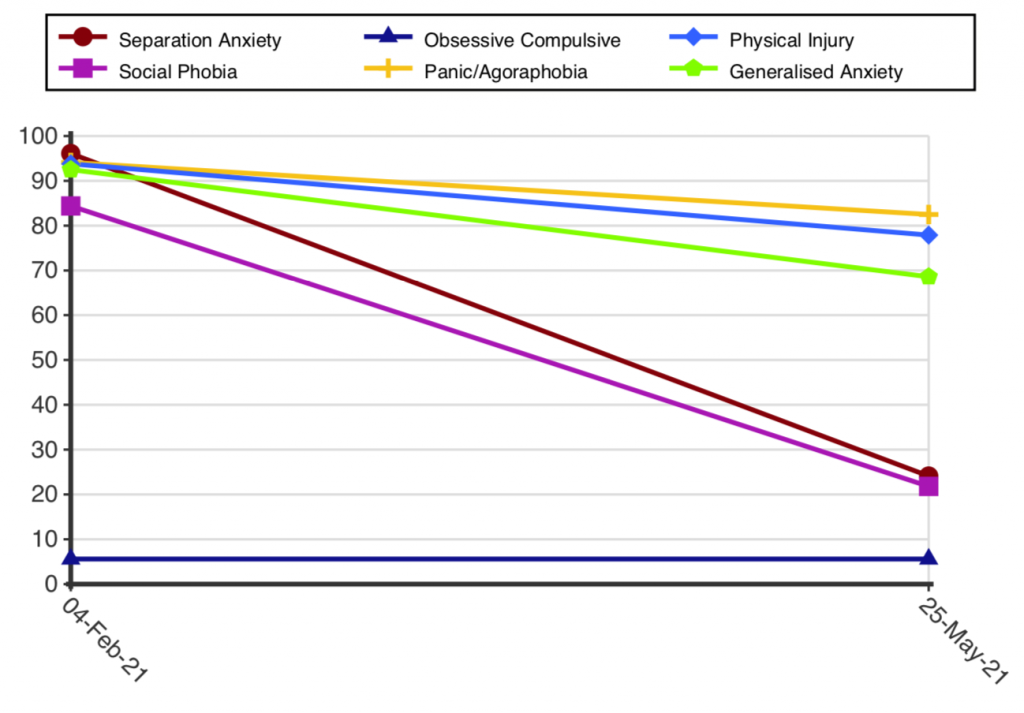
As many NovoPsych users know, increasing number of private psychology practices are engaging in monitoring outcomes. These practices are using outcome data to tender for contracts, provide feedback for professional development and service improvement, and occasionally publishing their results publicly and provided to consumers via a service’s website. These are positive developments that have occurred in the absence of policy incentives. In the future this can be further encouraged by linking extra levels of Medicare funding with the requirement for routine outcome monitoring. For example, increasing the limit of 10 psychology sessions to 20 per year, provided that the service provider uses an approved outcome monitoring and reporting framework.
Benchmarking treatment outcomes via routine outcome monitoring is an extremely valuable process. It can help service providers identify their strengths and weaknesses compared to their peers and modify practices when necessary. Understandably, comparing treatment outcomes through benchmarking can be anxiety producing for providers who may feel their competency is being scrutinized.
I’d therefore suggest that any attempt to widely implement benchmarking for Medicare-subsidised psychology services delivered in a private setting be lead from within the profession, with an emphasis on self-directed quality improvement. Education and training for clinicians on outcome monitoring and benchmarking practices is key and care should be taken to empower professionals who participate.
In due course standardized approaches to publishing outcome data for public consumption could be developed, providing more transparently when mental health consumers are making health care choices. In addition, outcome data could be a key component for accreditation standards developed from within the profession for psychology private practices.
The profession of psychology has a flourishing peer supervision culture, where fellow psychologists provide feedback and train each other. Benchmarking augmented with current supervision practices would be a powerful quality improvement practice and could be supported via funding for data-driven supervision training.
We also acknowledge the risk of unintended consequences if benchmarking is rolled out in the wrong way, such as gaming or resistance from service providers. If implemented in partnership with professional groups we think unintended consequences can be successfully minimized.
Conclusion
There is certainly a lot of momentum around outcome monitoring. Many practices are getting ahead of the game by integrating outcome measures into their practice already. Some people will resist, some will be proactive. Either way, there are interesting times ahead!
Dr Ben Buchanan
NovoPsych Co-founder and Director
NovoPsych.com.au
References:
Chung, J., & Buchanan, B. (2018). A Self‐Report Survey: Australian Clinicians’ Attitudes Towards Progress Monitoring Measures. Australian Psychologist, 54(1), 3-12
Delgadillo, J., de Jong, K., Lucock, M., Lutz, W., Rubel, J., Gilbody, S., … & O’Hayon, H. (2018). Feedback-informed treatment versus usual psychological treatment for depression and anxiety: a multisite, open-label, cluster randomised controlled trial. The Lancet Psychiatry, 5(7), 564-572.