This is the interview version of the WHODAS 2.0, which can be completed by a clinician for interviewing individuals 18 years of age and over. There is also a proxy version, which can be completed by a relative, carer, or friend, a self-report version, or a child and youth version (the WHODAS-Child)..
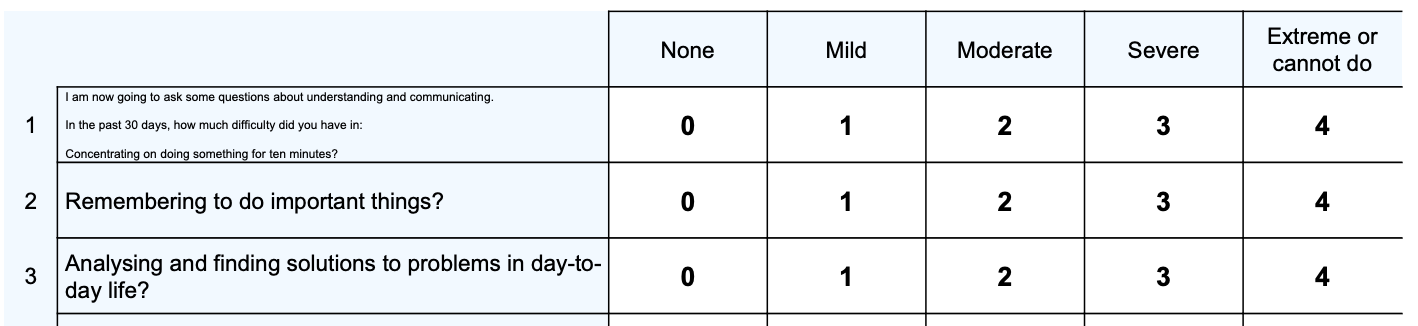
WHODAS 2.0 captures the level of functioning in six domains of life:
- Cognition – understanding and communicating
- Mobility – moving and getting around
- Self-care – attending to one’s hygiene, dressing, eating and staying alone
- Getting along – interacting with other people
- Life activities – domestic responsibilities, leisure, work and school
- Participation – joining in community activities, participating in society.
WHODAS 2.0 provides a common metric of the impact of any health condition in terms of functioning. Being a generic measure, the instrument does not target a specific disease – it can thus be used to compare disability due to different diseases. WHODAS 2.0 also makes it possible to design and monitor the impact of health and health-related interventions. The instrument has proven useful for assessing health and disability levels in the general population and in specific groups (e.g. people with a range of different mental and physical conditions). Furthermore, WHODAS 2.0 makes it easier to design health and health related interventions, and to monitor their impact.
Disability is a major health issue. When global assessments are made for burden of disease, more than half of the burden of premature mortality is due to overall disability. People generally seek health services because a disease makes it difficult for them to do what they used to do beforehand (i.e. because they are disabled) rather than because they have a disease. Health-care providers consider a case to be clinically significant when it limits a person’s daily activities, and they use disability information as the basis of their evaluation and planning.
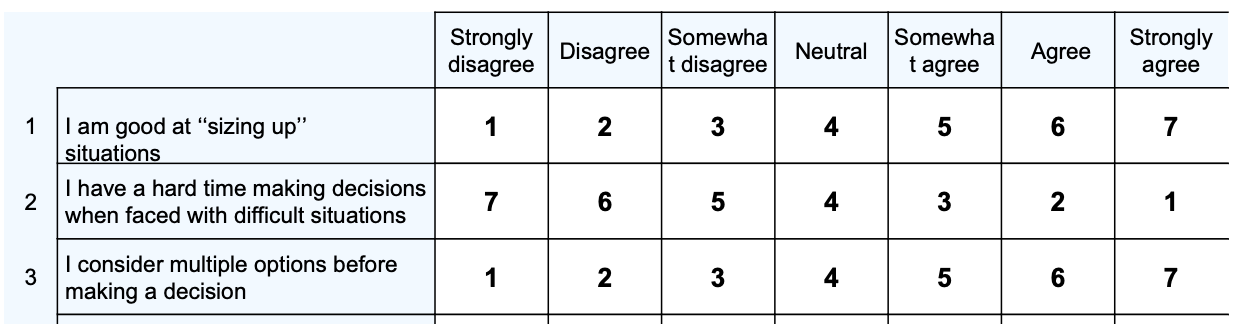
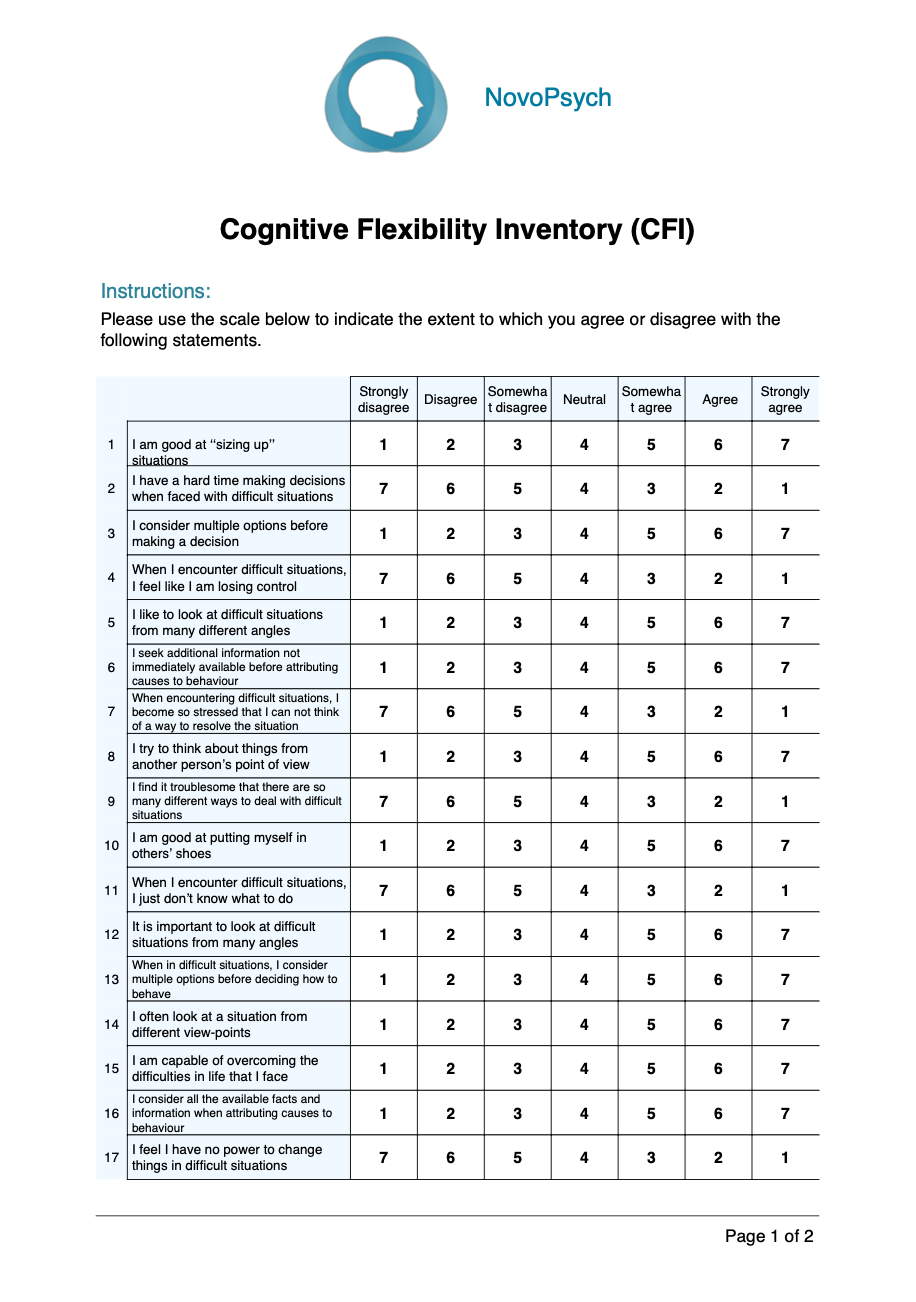
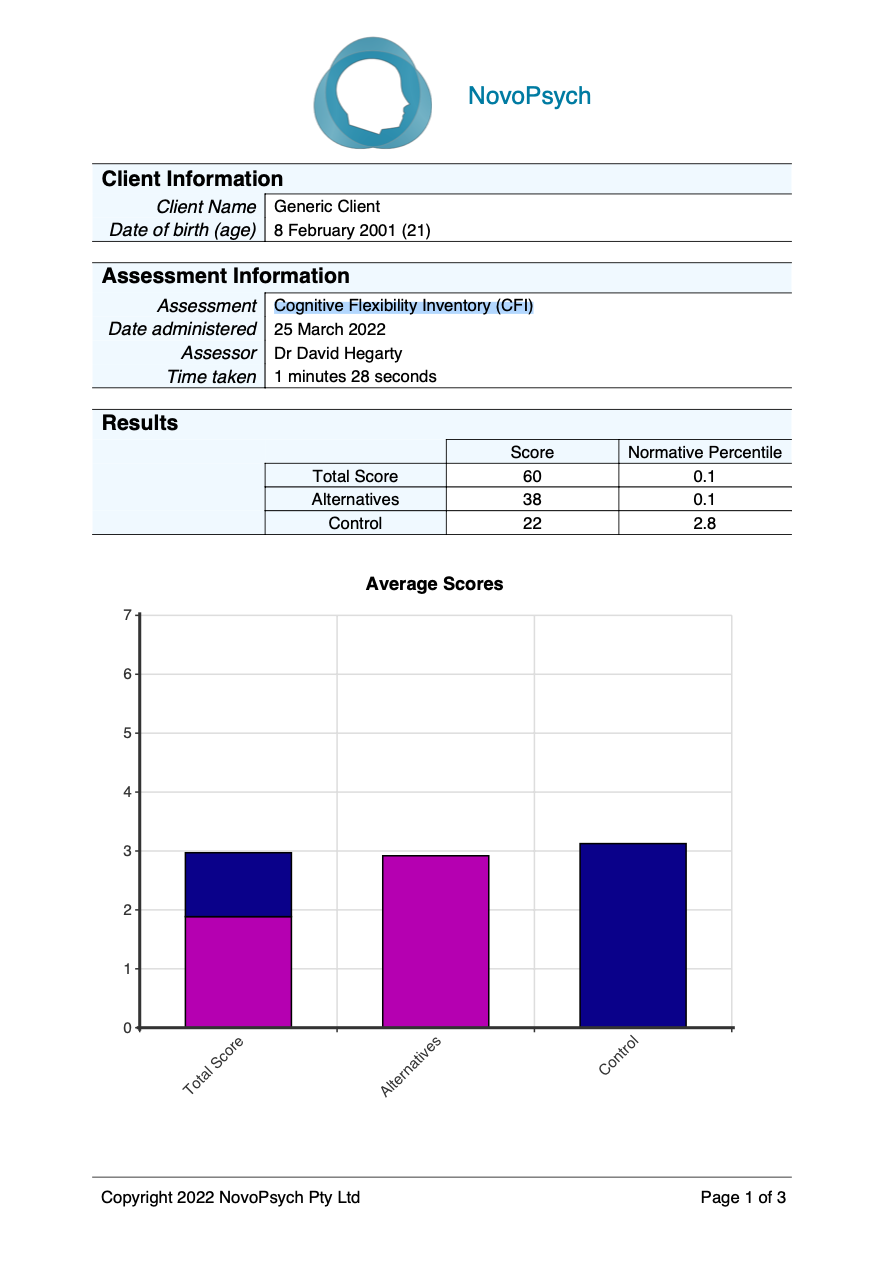
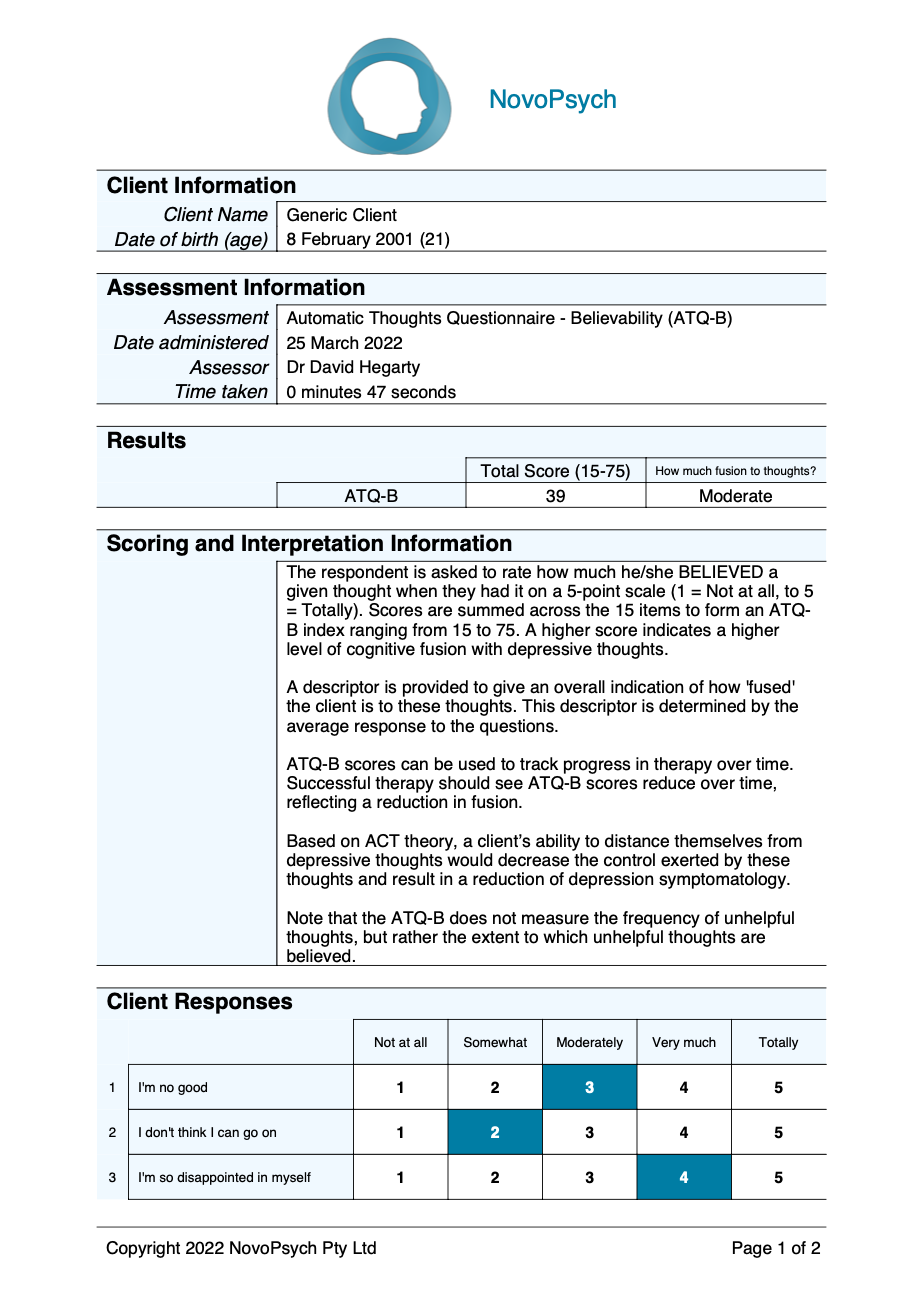
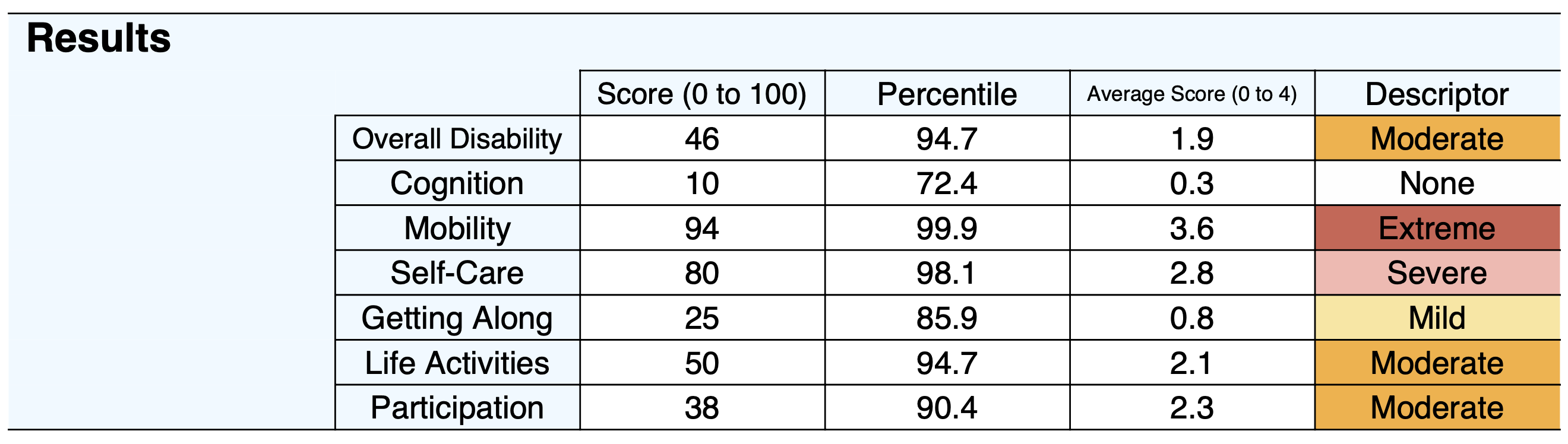
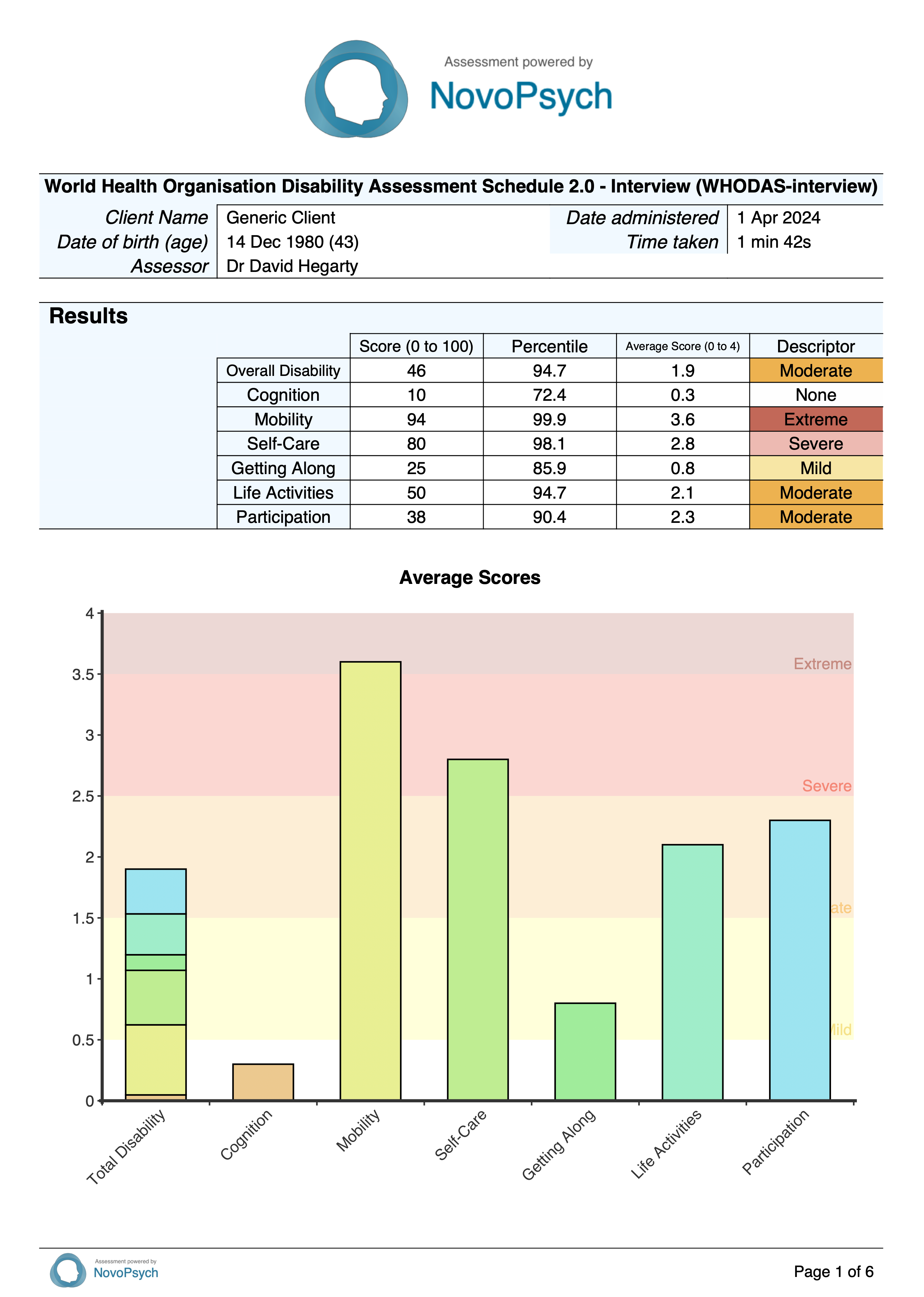
There are two scoring methods used for the WHODAS 2.0:
- Score (and its percentile)
- Average score (and its descriptor)
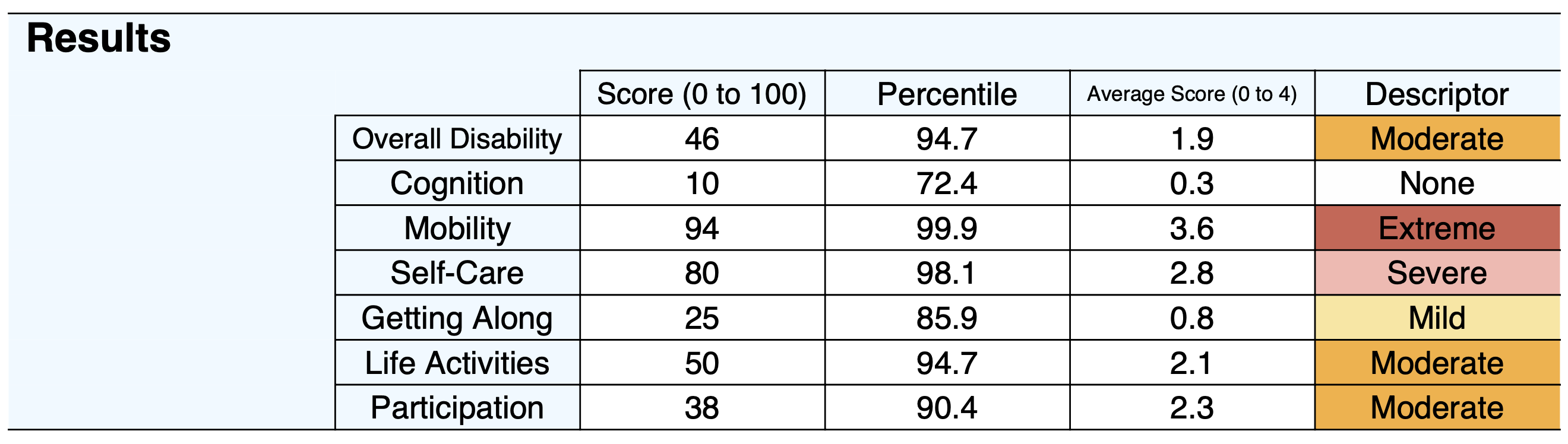
The first score is determined using “item-response-theory” (IRT), where it takes into account multiple levels of difficulty for each WHODAS 2.0 item (1-36). Converting the summary score into a metric ranging from 0 to 100 (where 0 = no disability; 100 = full disability). A percentile is provided that allows for a comparison to a large sample (n = 1,431) from a wide variety of populations (general population, populations with physical problems, populations with mental or emotional problems, populations with alcohol and drug use problems) from over 21 countries (WHO, 2010). A percentile of 50 indicates that an individual is experiencing an average level of disability when compared to other members of the sample.

The average scores are comparable to the WHODAS 5-point scale, which allows the clinician to think of the individual’s disability in terms of none (0-0.49), mild (0.5-1.49), moderate (1.5-2.49), severe (2.5-3.49), or extreme (3.5-4). The average domain score is calculated by dividing the raw domain score by the number of items in the domain. The average general disability score is calculated by dividing the raw overall score by number of items in the measure (i.e., 36). Average scores should be emphasised when the client misses optional items as its scoring caters for these missing items, whereas the complex scoring method does not.
The two scoring methods are used for each of the 6 domains:
- Cognition (q 1 – 6)– Assesses communication and thinking activities; specific areas assessed include concentrating, remembering, problem solving, learning and communicating.
- Mobility (q 7 – 11) – Assesses activities such as standing, moving around inside the home, getting out of the home and walking a long distance.
- Self-care (q 12 – 15) – Assesses hygiene, dressing, eating and staying alone.
- Getting along (q 16 – 20) – Assesses interactions with other people and difficulties that might be encountered with this life domain due to a health condition; in this context, “other people” includes those known intimately or well (e.g. spouse or partner, family members or close friends) and those not known well (e.g. strangers).
- Life activities (q 21 – 29; note, questions 26-29 are optional if not relevant) – Assesses difficulty with day-to-day activities (i.e. those that people do on most days, including those associated with domestic responsibilities, leisure, work and school).
- Participation (q 33 – 40) – Assesses social dimensions, such as community activities; barriers and hindrances in the world around the respondent; and problems with other issues, such as maintaining personal dignity.
If there is excessive variability (i.e., some extreme responses) within a domain score (NovoPsych 2024), it will be noted in the interpretive text. In these cases, it is recommended that the domain score be de-emphasised in favour of an examination of individual items to determine the client’s strengths and weaknesses.

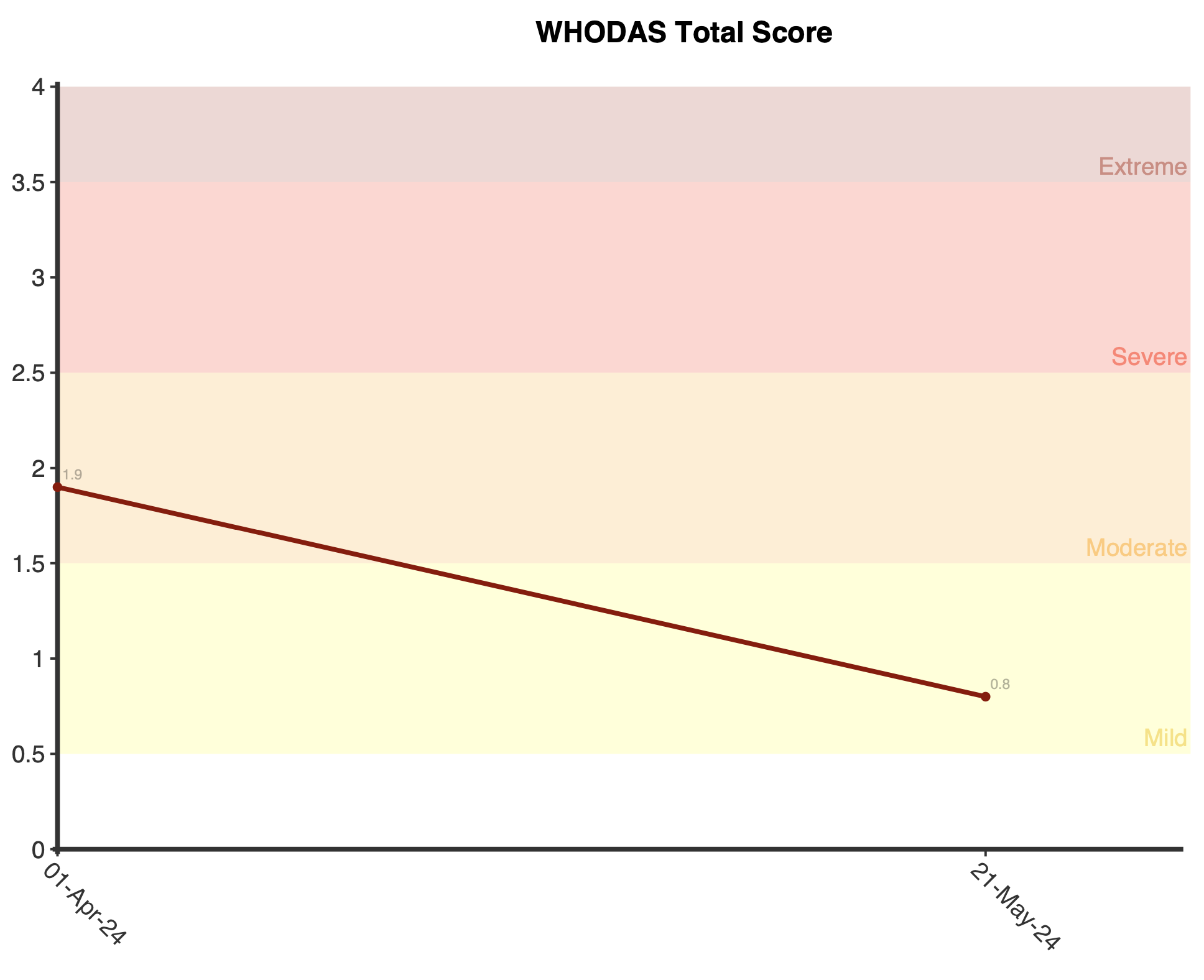
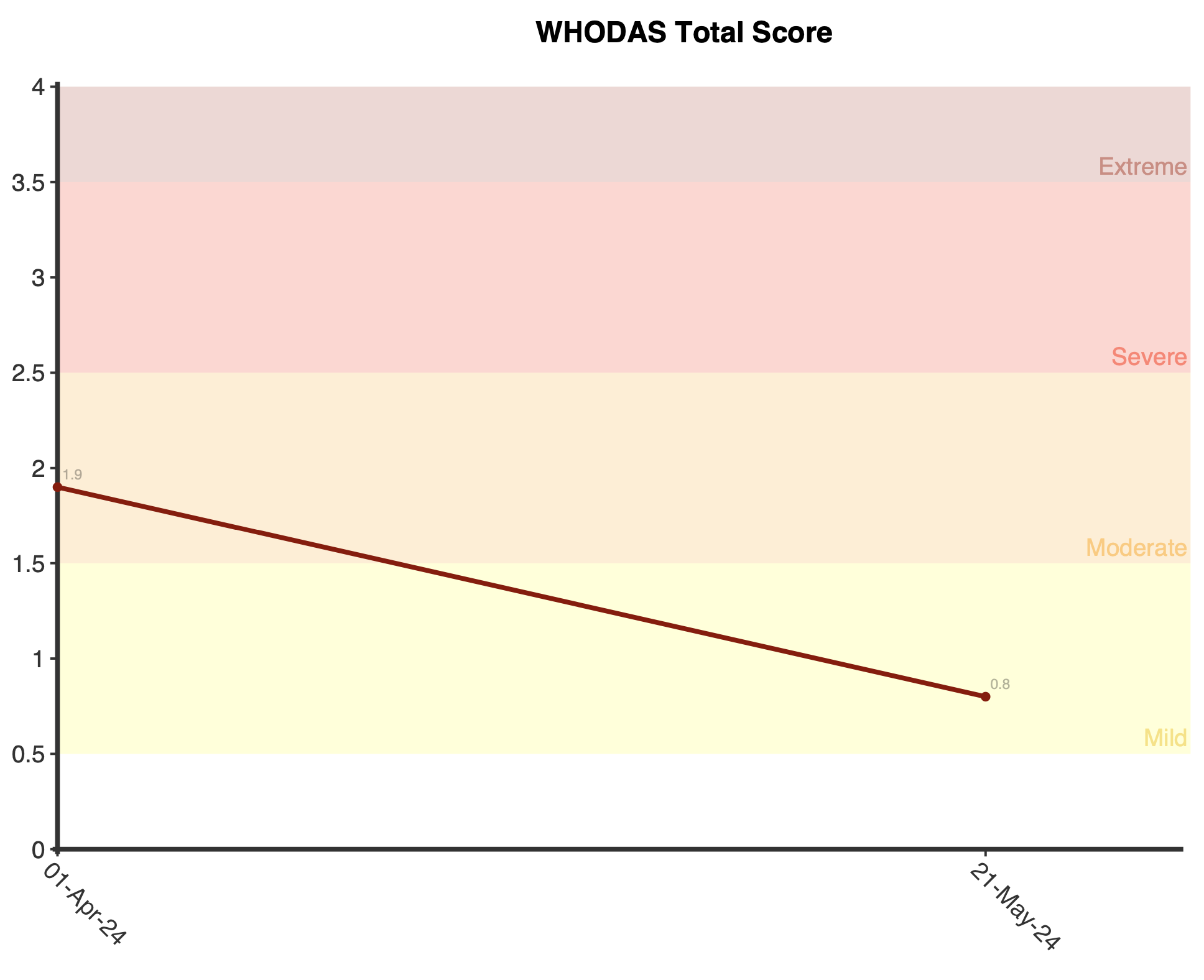
Plots are displayed upon first administration that shows the average scores for the total and domains. Upon multiple administrations of the WHODAS, longitudinal plots will be displayed for the total average score and for the domain average scores. This allows the practitioner to see if there has been any change in total and domain-level functioning for the client over time.
WHODAS 2.0 has excellent psychometric properties. Test–retest studies of the 36-item scale in countries across the world found it to be highly reliable, with an intra-class coefficient of 0.69–0.89 at item level; 0.93– 0.96 at domain level; and 0.98 at overall level. Cronbach’s alpha levels were generally very high (0.94 – 0.96 for domains and 0.98 for total score; WHO, 2010).
All items were selected on the basis of item-response theory and the instrument as a whole showed a robust factor structure that remained constant across cultures and different types of patient populations. Confirmatory factor analysis showed a rigorous association between the factor structure of the items and the domains, and between the domains and a general disability factor. These results support the unidimensionality of domains.
There are two scoring methods used for the WHODAS 2.0. The item response theory scoring method allows for more fine-grained analyses that make use of the full information of the response categories for comparative analysis across populations or subpopulations. The second scoring method simply uses the average score at the domain level, and while less advanced this scoring method was found to be reliable, easy to use, and clinically useful to the clinicians in the DSM-5 Field Trials (APA, 2021).
The validation studies also showed that WHODAS 2.0 compared well with other measures of disability or health status, and with clinician and proxy ratings. The WHODAS 2.0 shows sensitivity to change in people who have certain health conditions (e.g. cataract, hip or knee problems, depression, schizophrenia or alcohol problems), as it can pick up improvements in functioning following treatment.
To establish the validity of domain level interpretations, NovoPsych (2024) analysed data from over 3,000 responses for the WHODAS-interview that were completed between December 2021 and May 2024. Variability within the scores was analysed to determine the typical level of variability within each domain. Excessive variability that would render domain level scores difficult to interpret was defined as when there was a difference between the maximum and minimum score within a domain of greater than 2. This would mean that a response within a domain would have to have a minimum score of 0 (“None”) and a maximum score of 3 (“Severe”) or a minimum score of 1 (“Mild”) and a maximum score of 4 (“Extreme”) within the same domain to be classified as showing too much variability for domain level interpretation. Within the clinical data, the proportion of responses within each domain that exceeded the threshold for variability (based upon the above-mentioned criteria) was:
- Cognition: 24.3%
- Mobility: 28.7%
- Self-Care: 33.0%
- Getting Along: 39.6%
- Life Activities (optional school/work questions not completed): 3.8%
- Life Activities (all questions completed): 19.4%
- Participation: 38.5%
If a domain shows excessive variability then scores should be interpreted with caution. In particular, descriptors (mild, moderate, severe) at the domain level should be discounted in favour of an examination of individual responses to determine the specific abilities impacted by the condition.