The abbreviated Life Skills Profile (LSP-16; Rosen et al., 1989) is a clinician-rated assessment that contains 16 items which provide a key measure of function and disability for people with mental illness. The focus of LSP-16 is on the person’s general functioning, i.e. how the person functions in terms of their social relationships and ability to do day-to-day tasks.
The original Life Skills Profile (LSP) was developed by a team of clinical researchers (Rosen et al. 1989, Parker et al. 1991) as a brief, specific and jargon-free scale to assess a consumer’s abilities with respect to basic life skills. Work undertaken as part of the Australian Mental Health Classification and Service Costs (MH-CASC) study saw the 39 items reduced to 16. This reduction in item number aimed to minimise the rating burden on clinicians when the measure is used in conjunction with the Health of the NationOutcome Scale (HoNOS).
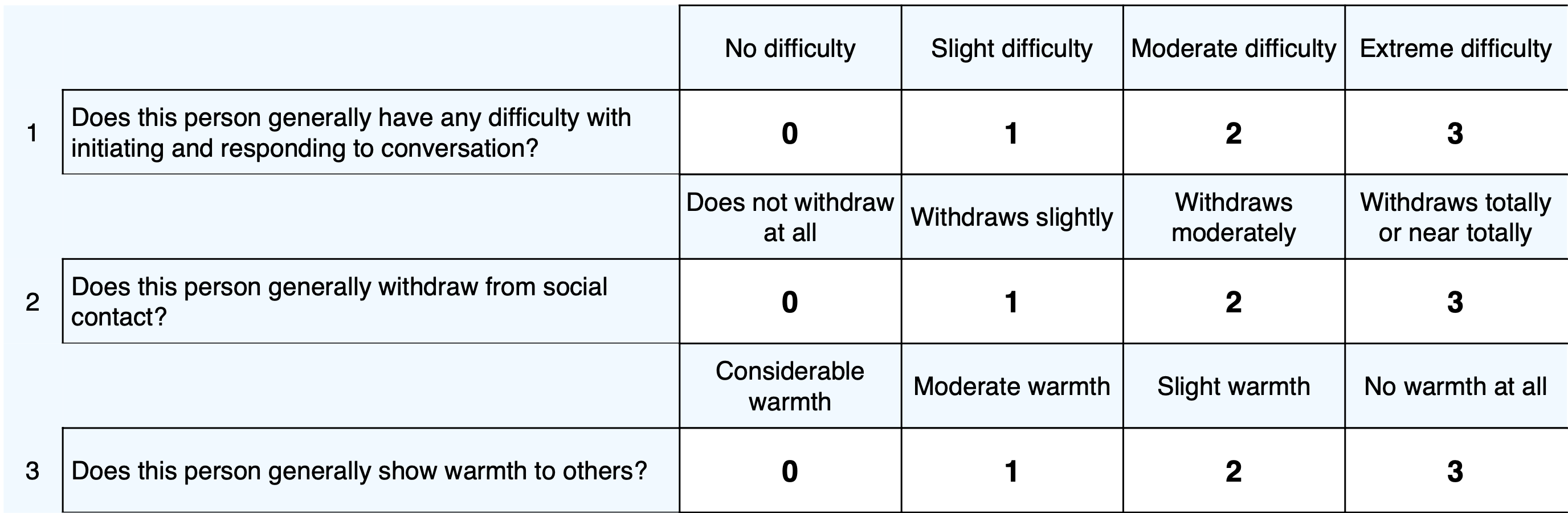
Example LSP-16 items:
There are four subscales assessed within the LSP-16:
Higher scores for the total score and subscale scores indicate a greater degree of disability. A total LSP scale score is calculated by adding individual scores for the whole scale together. Therefore, for the LSP-16, the total score can range from 0 to 48. As some items might not be relevant, items are optional and items with missing data are excluded from the calculation. An average score is provided for the total score and subscale scores so that comparisons can be made to determine relative areas of strength of challenges.
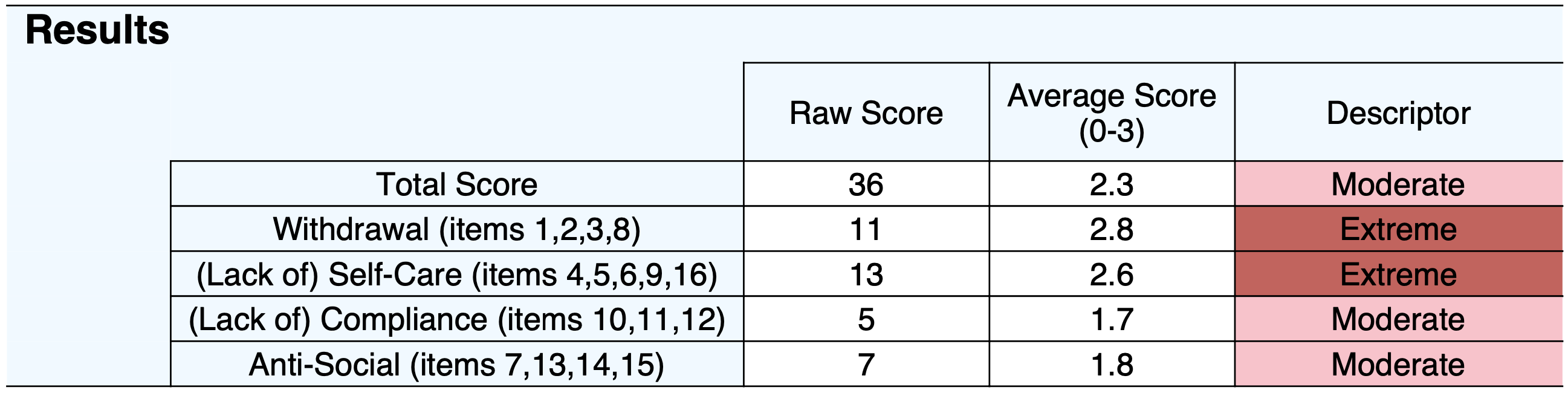
There are four subscales in the LSP-16:
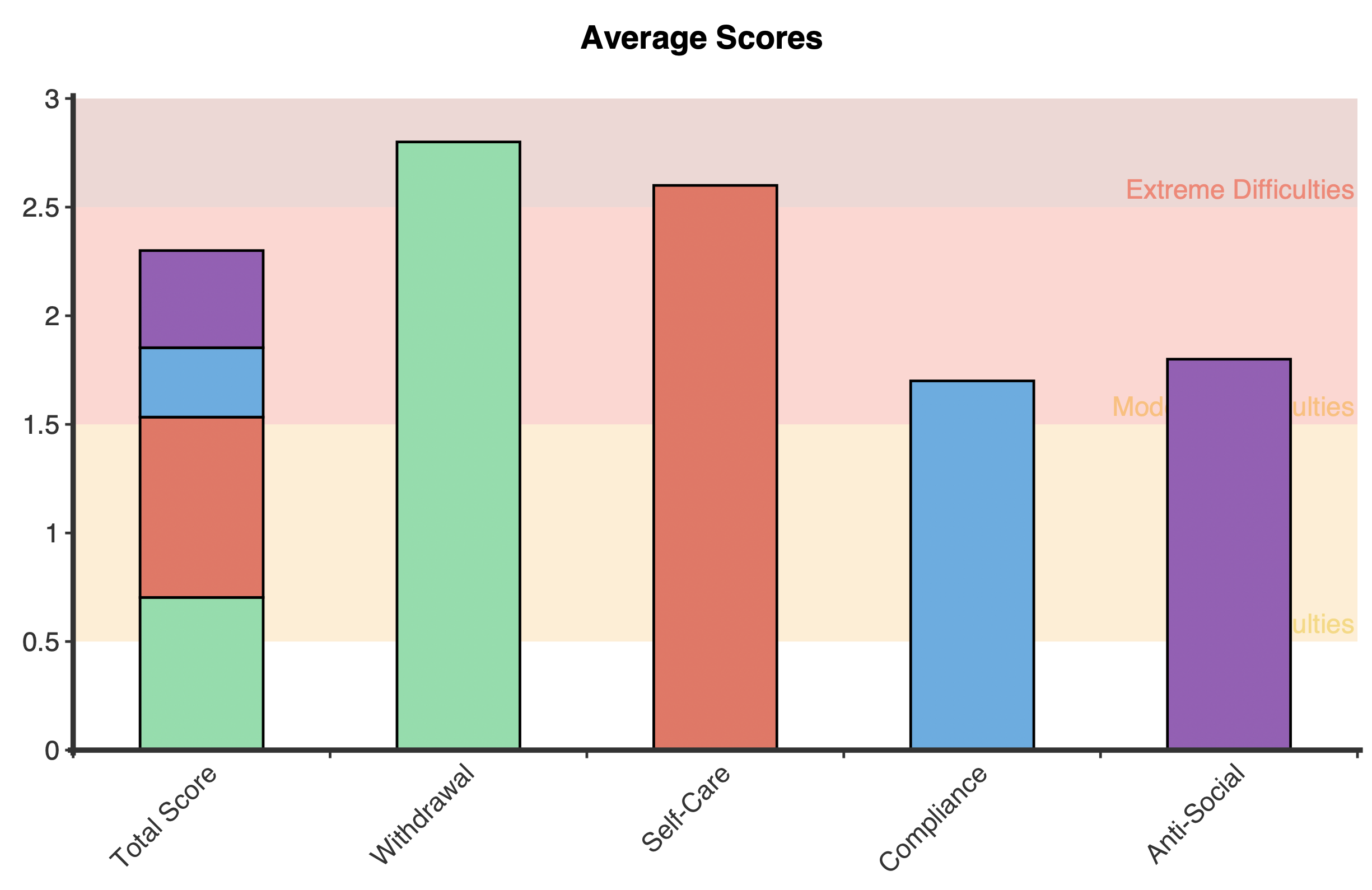
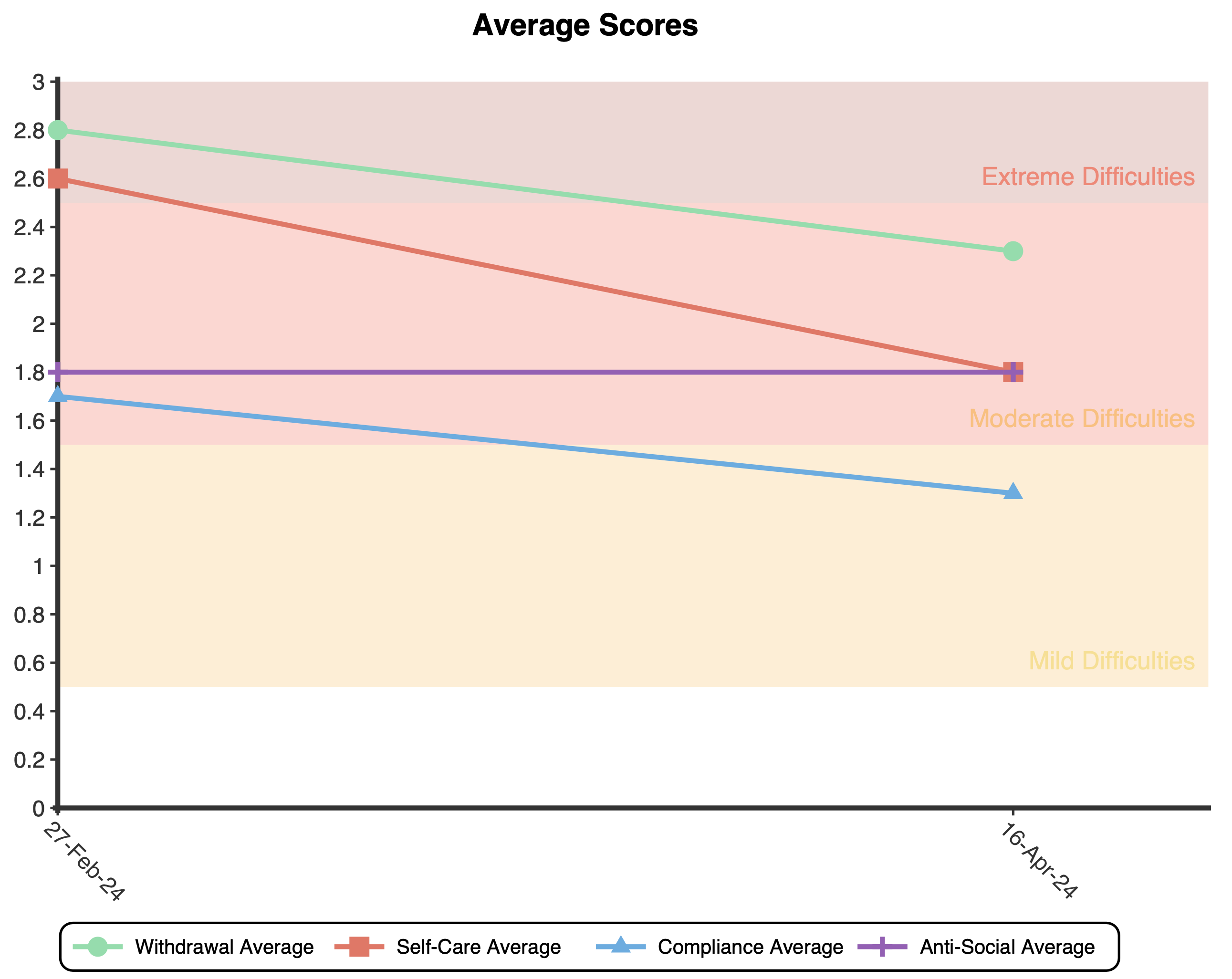
Plots are presented to show the average score for the first administration and multiple administrations of the LSP-16. The background colours on the plots match up to the response options on the LSP-16 to indicate what response category the average score is closest to (e.g., a score of 1.5 is closer to 2 and so is categorised as “moderate difficulties”).
Taken together, studies examining the psychometric properties of the LSP suggest that it has moderately good content, construct, concurrent and predictive validity; high test-retest and adequate inter-rater reliability; and good sensitivity to change. It also appears to demonstrate feasibility and utility in clinical settings.
A number of studies have examined the internal consistency of the LSP-39, as measured by Cronbach’s alpha. In these studies, the internal consistency has been reported as moderately high with subscale and total score alphas ranging from 0.64 to 0.88 (Parker et al., 1991; Rosen et al., 1989; Trauer et al., 1995) and 0.93 to 0.94 (Dickenson & Coursey, 2002; Trauer et al., 1995) respectively. The Communication subscale has been shown to have the poorest internal consistency (Parker et al., 1991; Rosen et al., 1989).
The LSP has been shown to perform well against the Health of the Nation Outcome Scales (HoNOS; Parker et al., 2002; Trauer et al., 2004; Wooff et al., 2003), the Katz Adjustment Scale (KAS; Parker et al., 1991), the Multnomah Communities Ability Scale (MCAS; Dickenson & Coursey, 2002), the Strauss-Carpenter Levels of Functioning Scale (LOF ; Dickenson & Coursey, 2002), the Global Assessment of Functioning Scale (GAF; Dickenson & Coursey, 2002; Parker et al., 2002; Simon et al., 2003), the Quality of Life Scale (QOL; Norman et al., 2000), 112 and the Global Assessment Scale (GAS; Wooff et al., 2003).
Rosen, A., Hadzi-Pavlovic, & D., Parker, G. (1989). The Life Skills Profile: A measure assessing function and disability in schizophrenia. Schizophrenia Bulletin. 15(2): 325-337. https://psycnet.apa.org/doi/10.1093/schbul/15.2.325
Dickinson, D. & Coursey, R.D. (2002). Independence and overlap among neurocognitive correlates of community functioning in schizophrenia. Schizophrenia Research. 56(1-2): 161- 170. https://doi.org/10.1016/s0920-9964(01)00229-8
Norman, R.M.G., Malla, A.K., McLean, T., et al. (2000). The relationship of symptoms and level of functioning in schizophrenia to general wellbeing and the Quality of Life Scale. Acta Psychiatrica Scandinavica. 102(4):303-309. https://doi.org/10.1034/j.1600-0447.2000.102004303.x
Parker, G., O’Donnell, M., Hadzi-Pavlovic, D., & Proberts, M. (2002). Assessing outcome in community mental health patients: A comparative analysis of measures. International Journal of Social Psychiatry. 48(1):11-19. https://doi.org/10.1177/002076402128783046
Parker, G., Rosen, A., Emdur, N., & Hadzi-Pavlovic, D. (1991). The Life Skills Profile: Psychometric properties of a measure assessing function and disability in schizophrenia. Acta Psychiatrica Scandinavica. 83(2): 145-152 https://doi.org/10.1111/j.1600-0447.1991.tb07381.x
Simon, A.E., Giaocomini, V., Ferrero, F., & Mohr, S. (2003). Dysexecutive syndrome and social adjustment in schizophrenia. Australian and New Zealand Journal of Psychiatry. 37(3):340- 346. https://doi.org/10.1046/j.1440-1614.2003.01186.x
Trauer, T., Duckmanton, R.A., & Chiu, E. (1995). The Life Skills Profile: A study of its psychometric properties. Australian and New Zealand Journal of Psychiatry. 29(3): 492-499. https://psycnet.apa.org/doi/10.3109/00048679509064959
Trauer, T., Eagar, K., Gaines, P., & Bower, A. (2004). New Zealand Mental Health Consumers and their Outcomes. Auckland: Health Research Council of New Zealand. https://www.researchgate.net/publication/265246873_New_Zealand_Mental_Health_Consumers_and_Their_Outcomes
Wooff, D., Schneider, J., Carpenter, J., & Brandon, T. (2003). Correlates of stress in carers. Journal of Mental Health. 12(1):29-40. https://doi.org/10.1080/09638230021000058274
NovoPsych’s mission is to help mental health services use psychometric science to improve client outcomes.
© 2023 Copyright – NovoPsych – All rights reserved