The Acceptance and Action Questionnaire – version 2 (AAQ-II), is the most widely used measure of psychological flexibility. It can be used weekly track how individuals are applying flexibility skills to their daily lives and is often used to measure progress in Acceptance and Commitment Therapy (ACT).
The AAQ-II defines psychological flexibility is defined as the ability to fully contact the present moment including all negative private events (which is thoughts, feelings, and physiological sensations) it contains, without needless defences and depending on the situation engaging or changing behaviours in line with goals and values (Bond et al., 2011). In contrast to this is psychological inflexibility which is the rigid dominance of psychological reactions over values and goals. This occurs when people fuse with negative thoughts and attempt to avoid experiencing unwanted private experiences. This avoidance has the ironic effect of increasing their distress, reducing their contact with the present moment, and reducing their likelihood of pursuing goals and values (Hayes et al., 2004). Note that different definitions of psychological flexibility are used in the neurocognitive literature.
Psychological inflexibility is purported to be determinant of psychological distress and behavioural ineffectiveness (Hayes et al., 2004; Bond et al., 2011). Therefore, greater levels of psychological inflexibility is associated with greater emotional distress (e.g. higher levels of depression and anxiety) and poorer life functioning (e.g. more absence from work).
A behaviour therapy that is focused on decreasing psychological inflexibility is Acceptance and Commitment therapy (ACT; Hayes et al., 2006). Studies have shown that ACT is effective in reducing depression and anxiety (e.g., Bohlmeijer, Fledderus, Rokx, & Pieterse, 2011; Forman et al., 2007) and chronic pain (e.g., Vowles & McCracken, 2008) and in increasing positive mental health (Fledderus, Bohlmeijer, Smit, & Westerhof, 2010). Meta-analyses have shown medium to large effect sizes of ACT interventions on different symptoms of psychological distress (Powers, Zum Vörde Sive Vörding, & Emmelkamp, 2009).
Higher total scores on the AAQ-II indicate higher psychological inflexibility, experiential avoidance, and more potential psychological distress. Lower total scores mean more psychological flexibility.
A normative percentile is also presented, comparing the respondent’s score against a sample of normative undergraduates and adults (Bond et al., 2011). A percentile of 50 indicates that the client has average (and healthy) levels of psychological flexibility and experiential avoidance. If the client scores 25 or above (percentile of approximately 86) then this is an indication that the client’s psychological inflexibility may impact their overall wellbeing. This ‘cutoff’ is indicated by a dotted line on the graphs.
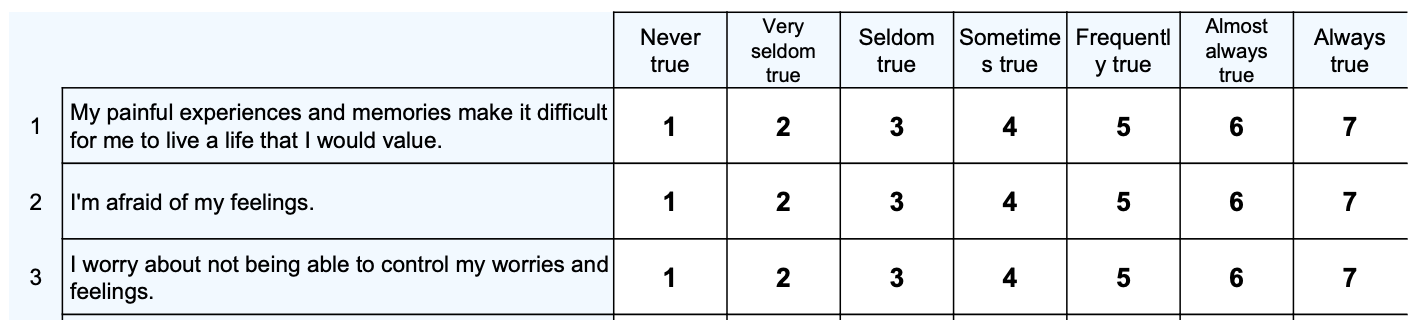
The AAQ-II was developed to address the short comings of the AAQ which had poor internal consistency. The AAQ-II items were generated by a panel of ACT experts from Australia, Europe and the United States. The items reflected either the likely dominance or non-dominance of private events (thoughts, feelings, and physiological sensations) in determining values directed action. The AAQ-II originally started out as a 10-item scale however after final psychometric analysis it was reduced to a 7-item scale (Bond et al., 2011).
Confirmatory factor analysis for the scale was conducted across 3 samples which included 433 undergraduate students from the University of Kentucky, 290 people who were seeking outpatient psychological help for Substance Abuse in New York City and 583 employees of a United Kingdom Bank – with a mean age of 34. Consistent results were seen across all 3 samples. The mean alpha coefficient was .84 (.78 – .88), and the 3- and 12-month test-retest reliability was .81 and .79, respectively.
Higher scores on the AAQ-II were associated with greater depression symptoms on the Beck Depression Inventory and the DASS and anxiety symptoms on the Beck Anxiety Inventory and the DASS. The sample who were seeking treatment for substance abuse were more psychologically inflexible (M = 28.34, SD = 9.92) than the samples that did not have that behavioural status (M = 18.51, SD = 7.05). This difference was statistically significant (F (1,3282) = 362.21, p < .000), with a very large effect size (d = 1.12) suggesting good predictive validity.
From the Bond et al. (2011) study, a normative sample was determined (n = 1,016) from the combination of an undergraduate student sample (n = 433) and an adult employee sample (n = 583). The mean for the total score of the AAQ-II was 18 (sd = 6.4). Given the Bond et al. (2011) findings and the relationship between AAQ-II scores and the BDI-II, GHQ, and GSI, a score of 1 standard deviation above the normative mean (approx. 25 or above) on the AAQ-II indicates psychological distress. These findings have recently been confirmed in a Brazilian normative sample, where a score of 25 or above would classify clients as moderate / severe on measures of anxiety and scores of 27 or above would classify clients as moderate / severe on measures of depression (Berta-Otero et al., 2023).
Bond, F. W., Hayes, S. C., Baer, R. A., Carpenter, K. M., Guenole, N., Orcutt, H. K., Waltz, T., & Zettle, R. D. (2011). Preliminary psychometric properties of the Acceptance and Action Questionnaire – II: A revised measure of psychological inflexibility and experiential avoidance. Behavior Therapy, 42, 676–688.
Berta-Otero, T., Barceló-Soler, A., Montero-Marin, J., Maloney, S., Pérez-Aranda, A., López-Montoyo, A., . . . Demarzo, M. (2023). Experiential avoidance in primary care providers: Psychometric properties of the Brazilian “Acceptance and action questionnaire” (AAQ-II) and its criterion validity on mood disorder-related psychological distress. International Journal of Environmental Research and Public Health, 20(1), 225. https://doi.org/10.3390/ijerph20010225
Bohlmeijer, E. T., Fledderus, M., Rokx, T. A. J. J., & Pieterse, M. E. (2011). Efficacy of an early intervention based on acceptance and commitment therapy for adults with depressive symptomatology: Evaluation in a randomized controlled trial. Behaviour research and therapy, 49(1), 62-67.
Fledderus, M., Bohlmeijer, E. T., Smit, F., & Westerhof, G. J. (2010). Mental health promotion as a new goal in public mental health care: A randomized controlled trial of an intervention enhancing psychological flexibility. American journal of public health, 100(12), 2372-2372.
Forman, E. M., Herbert, J. D., Moitra, E., Yeomans, P. D., & Geller, P. A. (2007). A randomized controlled effectiveness trial of acceptance and commitment therapy and cognitive therapy for anxiety and depression. Behavior modification, 31(6), 772-799.
Hayes, S. C., Strosahl, K. D., Wilson, K. G., Bissett, R. T., Pistorello, J., Toarmino, D., Polusny, M., A., Dykstra, T. A., Batten, S. V., Bergan, J., Stewart, S. H., Zvolensky, M. J., Eifert, G. H., Bond, F. W., Forsyth J. P., Karekla, M., & McCurry, S. M. (2004). Measuring experiential avoidance: A preliminary test of a working model. The Psychological Record, 54, 553-578.
Powers, M. B., Vörding, M. B. Z. V. S., & Emmelkamp, P. M. (2009). Acceptance and commitment therapy: A meta-analytic review. Psychotherapy and psychosomatics, 78(2), 73-80
Vowles, K. E., & McCracken, L. M. (2008). Acceptance and values-based action in chronic pain: a study of treatment effectiveness and process. Journal of consulting and clinical psychology, 76(3), 397.
NovoPsych’s mission is to help mental health services use psychometric science to improve client outcomes.
© 2023 Copyright – NovoPsych – All rights reserved