The Clinical Impairment Assessment questionnaire (CIA) is a 16-item self-report measure of the severity of psychosocial impairment due to eating disorder features (Bohn and Fairburn, 2008). It focuses on the past 28 days. It was developed as a measure of functional impairment in domains of life that are typically affected by an eating disorder which includes mood and perception of self, cognitive functioning, interpersonal functioning, and work performance. It has been normed in adults 17-65 years of age. The CIA is intended to assist in the clinical assessment of patients both before and after treatment for eating disorders (Bohn et al, 2008).
The purpose of this scale is to provide a simple single index of the severity of the psychosocial impairment secondary to eating disorder features. It has been designed to be completed immediately after filling in a measure of eating disorder features that covers the same time frame such as the Eating Disorder Examination questionnaire, EDE-Q (Fairburn and Beglin, 2008). The reason for this being that the patient has the eating disorder features “front of mind” when filling in the CIA (Bohn & Fairburn, 2008).
The creators of the CIA recognised that the psychopathology of eating disorders not only needs to evaluate the nature and severity of the eating disorder features but also the importance of assessing the impact of these features on their psychosocial and physical functioning (Bohn et al., 2008). Eating disorders have profound effects on one’s psychosocial functioning. An example of this being that these patients’ over-evaluation of shape and weight has a marked effect on their ability to form and maintain interpersonal relationships. The CIA was developed to measure the profoundly negative impacts that an ED can have on a patient’s life.
Scores range from 0 to 48, with higher ratings indicate a higher level of impairment. A global CIA score is calculated to measure the overall severity of secondary psychological impairment, by adding together items and prorating items if 12 of 16 items have been rated. A global score of 16 represents clinically significant impairment (Bohn et al., 2008).
Clinical percentiles ranks are also presented, showing the scores in comparison to people with eating disorders (Anorexia, Bulimia and Eating Disorder Not Otherwise Specified; Bohn et al., 2008). Higher percentiles indicate more impairment. Scores at or above the 38th percentile indicate clinically significant impairments (as defined by raw score = 16), and indicates that the respondent scored higher than 38 percentile of people with an eating disorder. This cutoff is represented by a dotted line on the graph.
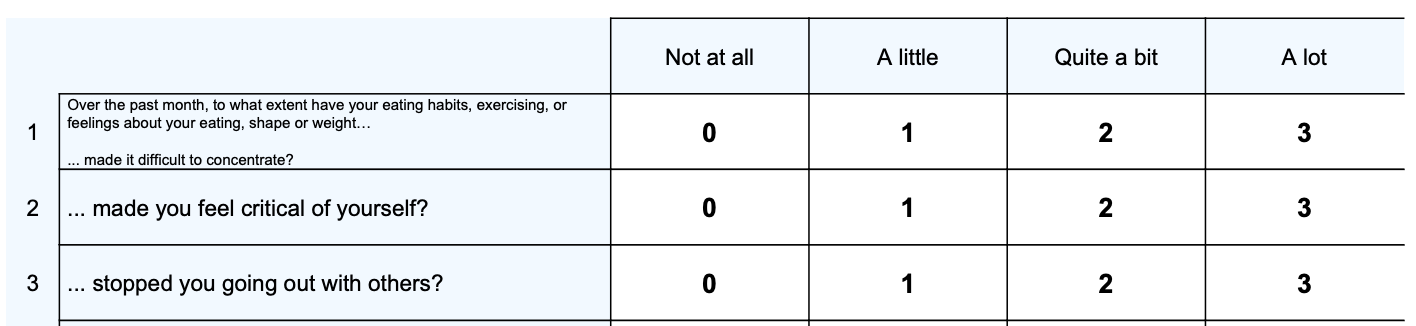
Three sub-scales are computed, representing different areas of impairment that can result from eating disorders:
– Personal impairment (Items 2, 8, 9, 11, 14, 16)
– Social impairment (items 3, 7, 10, 12, 15)
– Cognitive impairment (Items 1, 4, 5, 6, 13)
Note. Question 4 is optional and as the percentiles are based upon a complete score (with no missing items), if the client does not complete this question then the missing value is imputed by calculating the average of the total score or the cognitive impairment subscale (the two scores that depend on a value for question 4) and this value is added to provide a total and subscale total, respectfully. Although this imputation method will provide a valid result for these scores if question 4 is left blank, the scores and percentiles should then be interpreted with some caution.
The data for the CIA was collected from 123 of 170 patients who were participating in a transdiagnostic CBT trial based in two eating disorder clinics in the UK (Bohn et al., 2008). Participants for the study were included if they were 18-65 years old, had an eating disorder reviewed by an expert, and had a body mass index of between 16 and 40. Those with co-occurring clinical depression were excluded as their impairment might have been due to the depression rather than the eating disorder. Of the 123 patients included in the study, 8 had anorexia nervosa, 48 had bulimia nervosa, 67 had an eating disorder not otherwise specified.
Each patient underwent a research assessment at the beginning and end of their treatment, and at 20, 40, 60, 104 and 208 weeks post-treatment. At each point they completed the EDE-Q and, immediately afterwards the CIA. At the same time there was a trained research assistant who administered an interview designed to identify secondary functional impairment.
The Cronbach’s Alpha for the CIA was 0.97. The overall mean (SD) score was 20.1 (13.4) with a range of 0-47 (highest possible score is 48). For the test-retest reliability, the mean (SD) scores of the 16-item CIA at times 1 and 2 were 10.56 (7.58) and 9.02 (8.18).
The following means and SDs were found for the three subscales:
– Personal impairment M=10.2 (6.05)
– Social impairment M=5.36 (4.58)
– Cognitive impairment M=4.51 (4.0)
For construct validity, significant positive correlations were found between total scores on the 16-item CIA and scores on the EDE-Q (r = 0.89, p < 0.001) and the clinicians’ impairment ratings (r = 0.68, p < 0.001). These relationships were evident at each time point.
The best cut-off point was a total CIA score of 16, which had a sensitivity of 76% and specificity of 86% (Bohn et al., 2008).
Bohn, K., Doll, H. A., Cooper, Z., O’Connor, M., Palmer, R. L., & Fairburn, C. G. (2008). The measurement of impairment due to eating disorder psychopathology. Behaviour research and therapy, 46(10), 1105-1110.
Bohn K, & Fairburn CG. (2008). Clinical Impairment Assessment Questionnaire (CIA 3.0). In Fairburn CG. Cognitive Behavior Therapy and Eating Disorders. New York: Guilford Press.
Bohn, K., Doll, H. A., Cooper, Z., O’Connor, M., Palmer, R. L., & Fairburn, C. G. (2008). The measurement of impairment due to eating disorder psychopathology. Behaviour research and therapy, 46(10), 1105-1110.
Fairburn CG, & Beglin SJ. (2008). Eating Disorder Examination Questionnaire (6.0). In Fairburn CG. Cognitive Behavior Therapy and Eating Disorders. New York: Guilford Press.
Jenkins, P. E. (2013). Psychometric validation of the Clinical Impairment Assessment in a UK eating disorder service. Eating behaviors, 14(2), 241-243.
NovoPsych’s mission is to help mental health services use psychometric science to improve client outcomes.
© 2023 Copyright – NovoPsych – All rights reserved