The Montgomery-Asberg Rating Scale (MADRS) is a 10-item clinician-rated assessment for depression in adults (18+). The MADRS focusses more upon functional impairment and somatic symptoms than other assessments which might focus more upon depressive cognitive attitudes (Montgomery and Asberg, 1979).
The MADRS has been reported to be more sensitive to symptom changes over time compared to other assessments for depression (Carmody et al., 2006), so it can be a good assessment option to monitor client outcomes over time.
Retrospective research has shown that high scores on the MADRS have predicted suicide in depressed clients, above and beyond suicidal ideation and self-harm (Frekriksen et al., 2022), thus depression severity as measured by the MADRS independently correlates with suicide attempts.
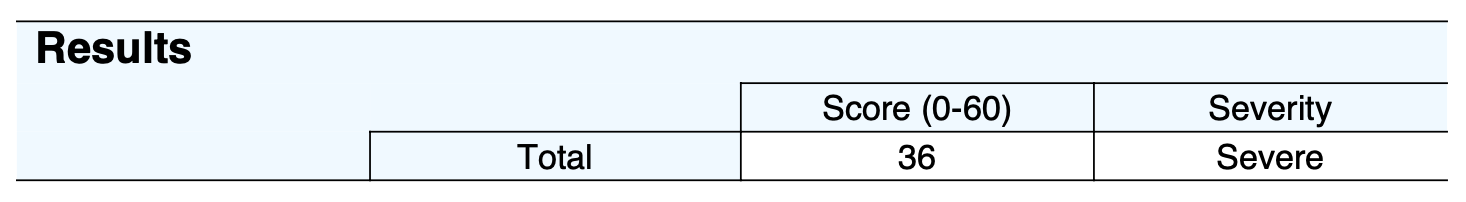
All items are summed to provide an overall score (from 0 to 60), with higher scores reflecting more severe depressive symptoms. A depression severity descriptor is also provided (Müller et al., 2003; Snaith et al., 1986; Thase et al., 2021):
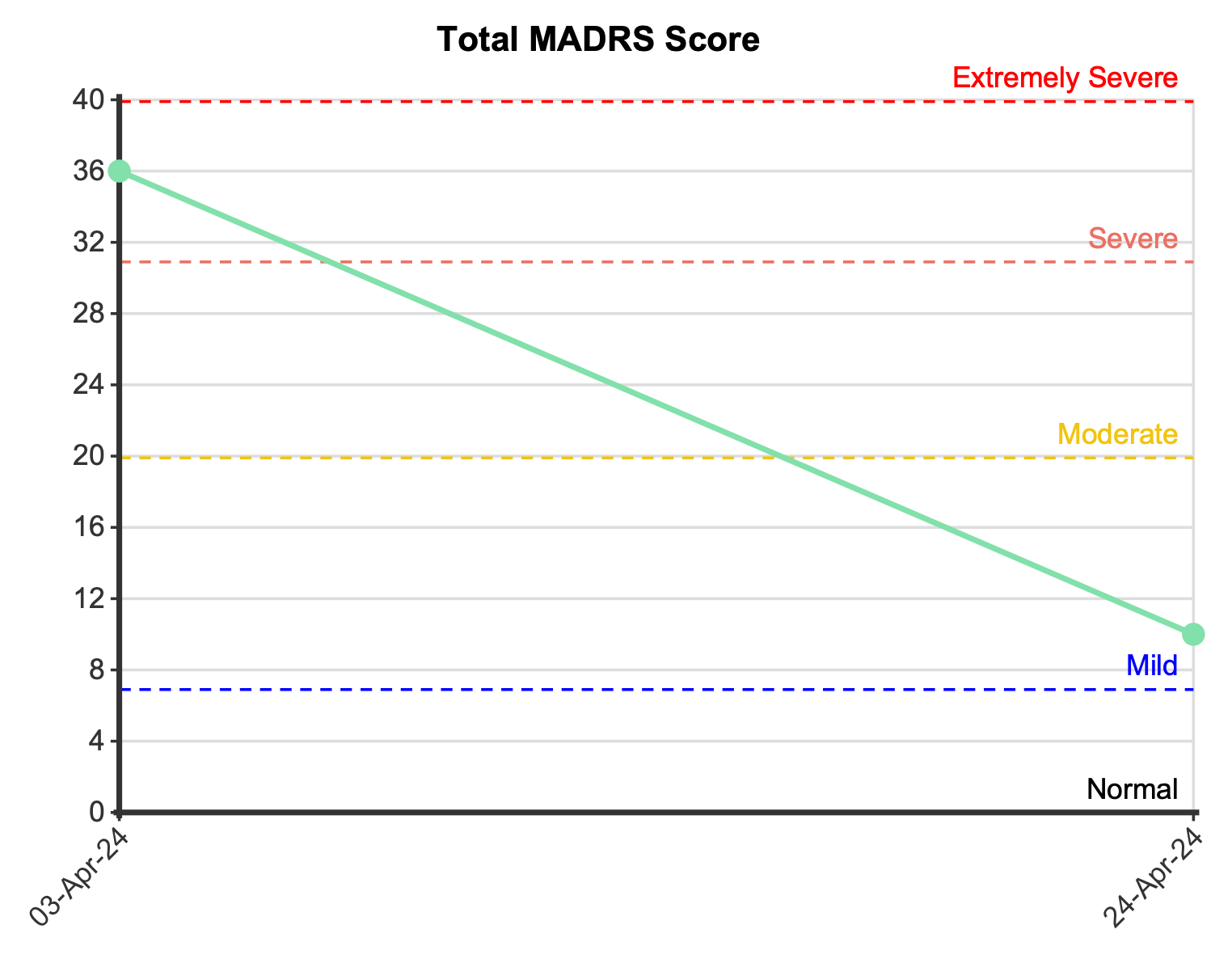
Upon multiple administrations of the MADRS, if the client improves by 6 points it will be noted as ‘clinically meaningful change’ or if the client improves by 12 points it will be noted as ‘clinically substantial change’ (Turkoz et al., 2020).
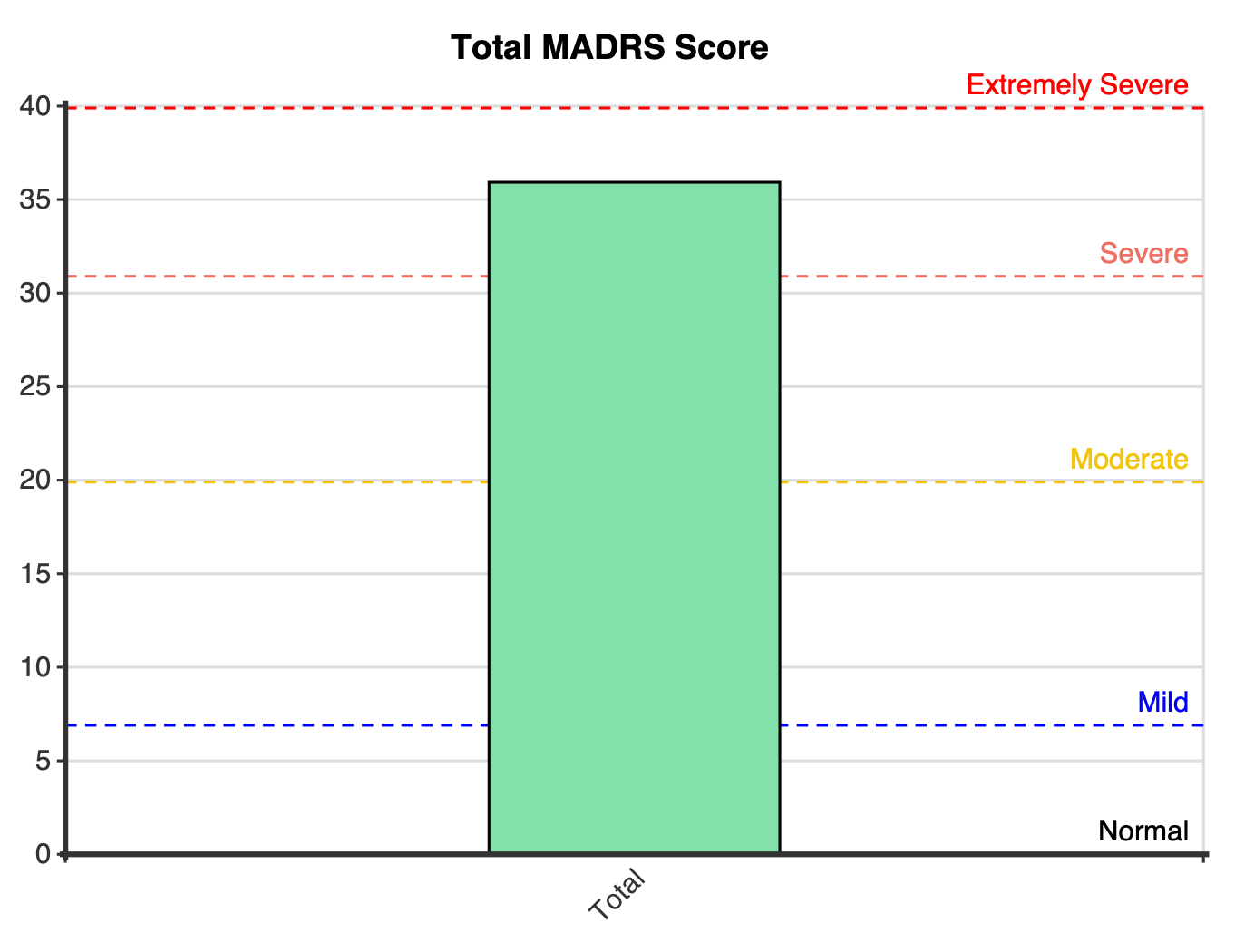
A plot is displayed for the first administration or multiple administrations of the MADRS with dotted lines indicating the severity cutoffs. Although the maximum score of the MADRS is 60, the y-axis may be truncated (dependent upon the client’s score/s) to enhance the readability of the plot.
The psychometric characteristics of the MADRS scale have undergone extensive scrutiny across various studies, with comparisons drawn to alternative scales such as the Hamilton Rating Scale for Depression (HRS). Notably, the MADRS exhibits robust internal consistency, marginally surpassing that of the HRS (Carmody et al., 2006). Clinician interrater reliability, both at the item level and for the total score, is very good (0.89 – 0.97; Montgomery & Asbert, 1979). Convergent validity is evident through a substantial correlation between MADRS scores and those from other measures like the HRS (r = 0.87 – 0.94; Carmody et al., 2006; Davidson et al., 1986; Heo et al. ,2007; Muller et al., 2003). The MADRS further exhibits a noteworthy ability to discriminate between various levels of depression severity (Carmody et al., 2006). Studies consistently highlight the MADRS’s heightened sensitivity to treatment-related changes (Davidson et al., 1986; Mulder et al., 2003).
Although cutoffs were derived by Snaith et al. (1986), subsequent research by Müller et al. (2003) modified the cutoff between moderate and severe to 31 (sensitivity 92%, specificity 83%) and research by Thase et al. (2021) added a further description at the top end of the scale (40 – 60). Although the work by Thase et al. (2021) was focussed upon bi-polar patients and added significantly more descriptors (although still similar to Snaith et al.’s cutoffs and descriptors), for simplicity’s sake it was decided to keep the prior descriptors but simply add the descriptor for ‘extremely’ at the top end.
As determined by Turkoz et al. (2020), a clinically meaningful change score (as determined by a one point change in the Clinical Global Impression – Severity (CGI-S) score) on the MADRS is 6 points and a clinically substantial change (a two point change in CGI-S) score is 12 points.
Montgomery, S.A., & Asberg, M. (1979). A new depression scale designed to be sensitive to change. British Journal of Psychiatry, 134(4), 382–389. doi: 10.1192/bjp.134.4.382. PMID: 444788.
Carmody, T.J., Rush, A.J., Bernstein, I., Warden, D., Brannan, S., Burnham, D., et al. (2006). The Montgomery Äsberg and the Hamilton ratings of depression: a comparison of measures. European Journal of Neuropsychopharmacology, 16(8), 601–611. doi: 10.1016/j.euroneuro.2006.04.008. Epub 2006 Jun 12. PMID: 16769204; PMCID: PMC2151980.
Davidson, J., Turnbull, C.D., Strickland, R., Miller, R., & Graves, K. (1986). The Montgomery-Asberg Depression Scale: reliability and validity. Acta Psychiatry Scandinavica, 73(5), 544–548. doi: 10.1111/j.1600-0447.1986.tb02723.x. PMID: 3751660.
Fredriksen, K. J., Gjestad, R., Walby, F. A., Anda, L. G., Oedegaard, K. J., & Schoeyen, H. K. (2022). High Scores on the Montgomery-Åsberg Depression Rating Scale and Psychotic Symptoms Predict Suicide: A Prospective Cohort Study of Psychiatric Acute Ward Patients. The Journal of Clinical Psychiatry, 83(5), 41950. https://doi.org/10.4088/JCP.21m14018
Heo, M., Murphy, C.F., & Meyers, B.S. (2007). Relationship between the Hamilton Depression Rating Scale and the Montgomery-Åsberg Depression Rating Scale in depressed elderly: a meta-analysis. American Journal of Geriatric Psychiatry, 15(10), 899–905. doi: 10.1097/JGP.0b013e318098614e. PMID: 17911366.
Mulder, R.T., Joyce, P.R., & Frampton, C. (2003). Relationships among measures of treatment outcome in depressed patients. Journal of Affective Disorders, (1–3), 127–135. doi: 10.1016/s0165-0327(02)00080-0. PMID: 12943942.
Müller, M. J., Himmerich, H., Kienzle, B., & Szegedi, A. (2003). Differentiating moderate and severe depression using the Montgomery-Asberg depression rating scale (MADRS). Journal of Affective Disorders, 77(3), 255–260. https://doi.org/10.1016/s0165-0327(02)00120-9
Snaith, R., Harrop, F., Newby, D., & Teale, C. (1986). Grade Scores of the Montgomery—Åsberg Depression and the Clinical Anxiety Scales. British Journal of Psychiatry, 148(5), 599-601. doi:10.1192/bjp.148.5.599
Fredriksen, K. J., Gjestad, R., Walby, F. A., Anda, L. G., Oedegaard, K. J., & Schoeyen, H. K. (2022). High Scores on the Montgomery-Åsberg Depression Rating Scale and Psychotic Symptoms Predict Suicide: A Prospective Cohort Study of Psychiatric Acute Ward Patients. The Journal of Clinical Psychiatry, 83(5), 41950. https://doi.org/10.4088/JCP.21m14018
Thase, M. E., Harrington, A., Calabrese, J., Montgomery, S., Niu, X., & Patel, M. D. (2021). Evaluation of MADRS severity thresholds in patients with bipolar depression. Journal of Affective Disorders, 286, 58–63. https://doi.org/10.1016/j.jad.2021.02.043
Turkoz, I., Alphs, L., Singh, J., Jamieson, C., Daly, E., Shawi, M., Sheehan, J. J., Trivedi, M. H., & Rush, A. J. (2021). Clinically meaningful changes on depressive symptom measures and patient-reported outcomes in patients with treatment-resistant depression. Acta Psychiatrica Scandinavica, 143(3), 253–263. https://doi.org/10.1111/acps.13260
NovoPsych’s mission is to help mental health services use psychometric science to improve client outcomes.
© 2023 Copyright – NovoPsych – All rights reserved