The Regensburg Insomnia Rating Scale (RIS) is a 10-item rating scale to assess the cognitive, behavioural, and emotional aspects of psychophysiological insomnia (PI; Crönlein et al., 2013). The scale has been validated in an adult population.
Psychophysiological insomnia is a form of primary insomnia and is defined by International Classifications of Sleep Disorders (ICSD-2) as a state of “heightened arousal and learned sleep preventing associations that result in a complaint of insomnia and associated decreased functioning during wakefulness.”
The specific criteria include difficulty in initiating or maintaining sleep, waking up too early, or sleep that is non-restorative or of poor quality. The sleep difficulties described above occur despite ample opportunity and circumstances for sleep, the symptoms are present for at least 1 month, and there is evidence of conditioned sleep difficulty and/or heightened arousal in bed (Perlis, and Gehrman, 2013).
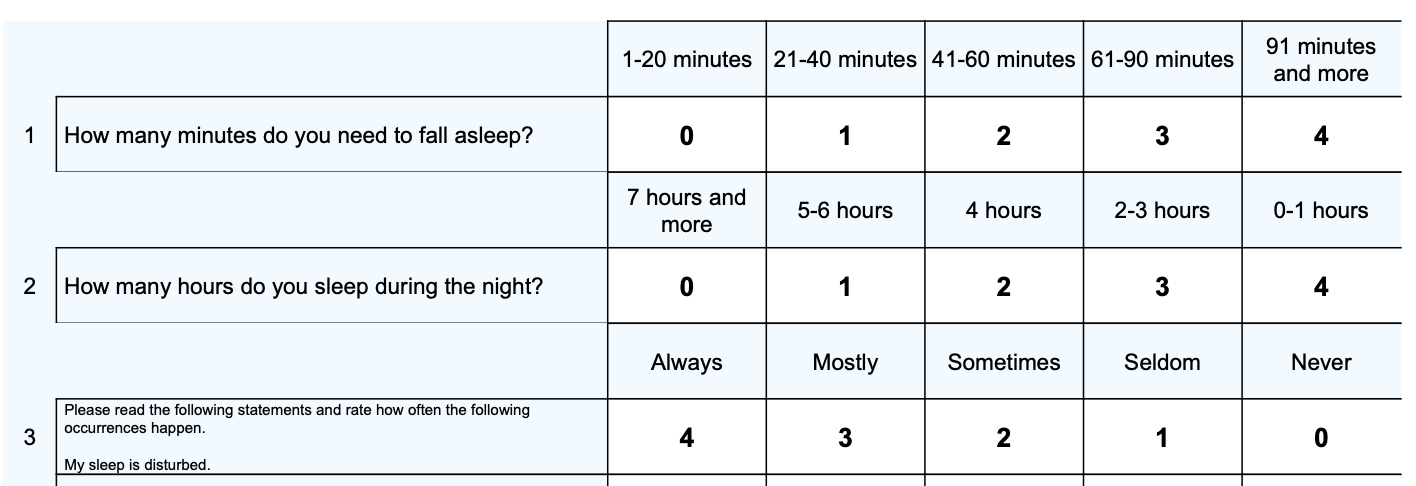
There have been several tools developed for the assessment of insomnia, however many do not target the psychological symptoms of insomnia or are too specific for routine clinical screening, as they measure only certain symptoms of insomnia such as pre-sleep worrying or one’s arousal state before sleep. The RIS was developed as a short scale that covers both the quantitative and qualitative aspects of sleep. It also measures four factors of sleep:
1. Poor Sleep Depth
2. Poor Sleep Quantity
3. Fearful Focus on Insomnia
4. Hypnotics and Poor Daytime Functioning
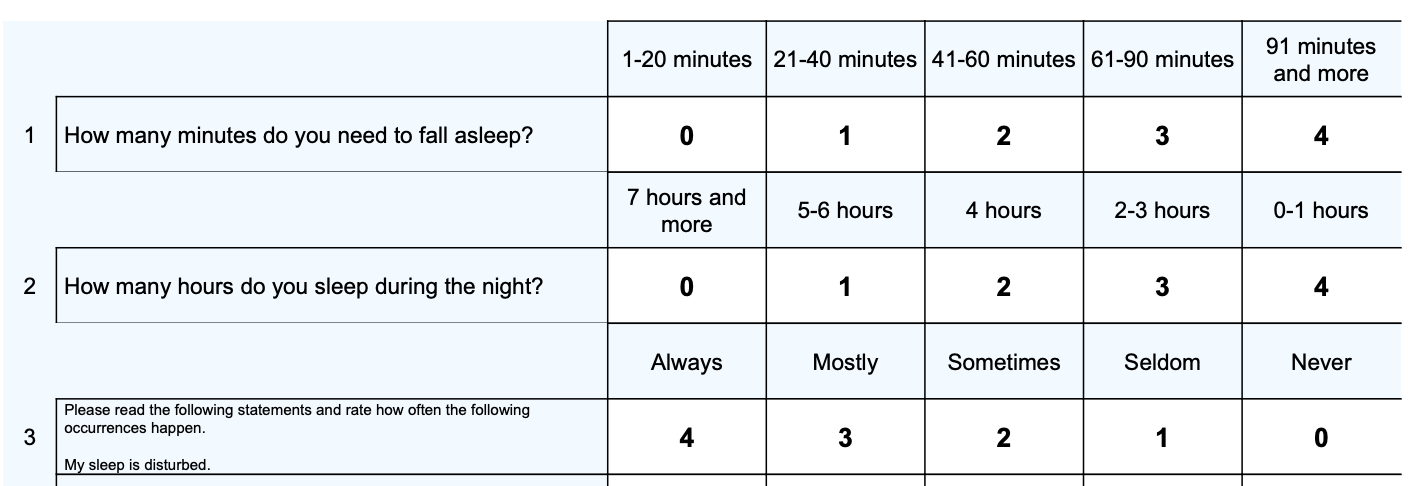
Total scores range from 0 to 40 points with higher scores indicative of more cognitive, behavioural, and emotional difficulties consistent with psychophysiological insomnia. Scores from 0-12 are considered normal and scores above the cutoff (13+) are indicative of symptoms consistant with psychophysiological insomnia that warrant further investigation.
A clinical percentile is shows a comparison of the total score of the respondent’s in comparison to patients with diagnosed psychophysiological insomnia (Cronlein et al., 2013). A clinical percentile of around 50 indicated that a client has scored at the average level for the clinical comparison group and would be indicative of significant cognitive, behavioural, and emotional symptoms consistent with psychophysiological insomnia.
There are four factors for the RSI:
1. Poor Sleep Depth (items 3, 4, 5) – measuring sleep continuity, easy awakening, and early awakening.
2. Poor Sleep Quantity (items 1, 2, 6) – measuring sleep latency, sleep duration, and sleepless nights.
3. Fearful Focus on Insomnia (items 7, 8) – measuring thinking about sleep and fear of insomnia.
4. Hypnotics and Poor Daytime Functioning (items 9, 10) – measuring impaired daytime fitness and hypnotics intake.
Average scores are presented for the four factors so that a comparison can be made (due to different numbers of questions in each factor) and which allows a comparison of relative strengths and weaknesses in the sleep factor areas (with higher average scores indicating more difficulties).
The RIS can be used to monitor the effectiveness of sleep interventions such as CBT-i.
The RIS was originally designed in Germany, where sleep experts compiled a list of typical complaints of psychophysiological insomnia (PI) patients, with emphasis put on the exact wording – such as “I wake up from the slightest sound.” To identify the items that were specific to PI, the list was given to patients with sleep apnoea (N=33), PI (N=36) and healthy controls (N=29; Cronlein et al., 2013). Items that did not discriminate between PI patients and the other two groups were excluded. From the items that remained, the list was further shortened to cover both qualitative and quantitative sleep parameters in a short scale.
After the RIS was constructed, the psychometric properties were investigated in two separate samples of patients with PI, one sample was used for the normative data, and the second group were tested pre and post cognitive behaviour therapy for insomnia (CBT-i; Cronlein et al., 2013). The inclusion criteria for this study was a diagnosis of PI irrespective of the use of hypnotics. Exclusion criteria was current or past continuous shift work, and a current severe physical or mental disorder that had a major influence on sleep. To assess specificity and sensitivity, a sample of 94 healthy controls was also included. The Normative Group, consisted of 218 PI patients with a mean age of 48.9, and mean duration of insomnia symptoms of 9.5 years. All patients were seeking help in a specialised sleep centre. The therapy group consisted of 38 PI patients who participated in a standardised CBT-i group.
The mean total RIS score for the sample was 22.6 with a standard deviation of 5.19, which was significantly higher than the score of the control group.
A RSI cut-off score of more than 12 has a sensitivity was 97.7% for PI patients and specificity was 97.9% for the healthy control sample. Cronbach’s Alpha was .89 for the whole sample. There was high concurrent validity with the Pittsburgh Sleep Quality Index (PSQI). The RIS is sensitive to improvements after CBT-i, with all items improving except “sleep duration”.
Cronlein et al. (2013) found that there were four factors for the RSI:
1. Poor Sleep Depth – 20% of the variance
2. Poor Sleep Quantity – 19% of the variance
3. Fearful Focus on Insomnia – 15% of the variance
4. Hypnotics and Poor Daytime Functioning – 12% of the variance
Crönlein, T., Langguth, B., Popp, R., Lukesch, H., Pieh, C., Hajak, G., & Geisler, P. (2013). Regensburg Insomnia Scale (RIS): a new short rating scale for the assessment of psychological symptoms and sleep in insomnia; study design: development and validation of a new short self-rating scale in a sample of 218 patients suffering from insomnia and 94 healthy controls. Health and quality of life outcomes, 11(1), 1-8.
Crönlein, T., Langguth, B., Popp, R., Lukesch, H., Pieh, C., Hajak, G., & Geisler, P. (2013). Regensburg Insomnia Scale (RIS): a new short rating scale for the assessment of psychological symptoms and sleep in insomnia; study design: development and validation of a new short self-rating scale in a sample of 218 patients suffering from insomnia and 94 healthy controls. Health and quality of life outcomes, 11(1), 1-8.
Perlis, M., & Gehrman, P. (2013). Psychophysiological insomnia. the behavioural model and a neurocognitive perspective, 1997, 6.
Morin CM. Insomnia: Psychological assessment and management: Guilford press; 1993.
NovoPsych’s mission is to help mental health services use psychometric science to improve client outcomes.
© 2023 Copyright – NovoPsych – All rights reserved