The Difficulties in Emotion Regulation Scale (DERS) is a 36-item a measure designed to assess clinically relevant difficulties in emotion regulation. The DERS provides valuable insights into an individual’s ability to understand, accept, and manage emotions effectively.
The DERS was developed based on an integrative theoretical framework that conceptualises emotion regulation as involving: (a) awareness and understanding of emotions, (b) acceptance of emotions, (c) ability to engage in goal-directed behaviour and control impulsive behaviours when experiencing negative emotions, and (d) access to effective emotion regulation strategies (Gratz & Roemer, 2004).
The scale has been used with groups as young as 13 years old, but was originally validated in an adult population (Gratz & Roemer, 2004; Monell et al., 2020).
The scale consists of six subscales:
Research has shown that difficulties in emotion regulation as measured by the DERS may serve as a transdiagnostic risk factor across multiple forms of psychopathology (Skutch et al., 2019). The scale has demonstrated relationships with borderline personality disorder, posttraumatic stress disorder, anxiety disorders, substance use disorders, depression, and eating disorders (Sörman et al., 2022).
The DERS is a useful tool for formulation and treatment planning at the outset of therapy, as well as being suitable for repeated administrations for outcome monitoring. By identifying specific domains of emotion regulation challenges, the DERS can help clinicians target interventions, such as mindfulness techniques to improve emotional awareness, or building adaptive coping skills to regulate emotional states.
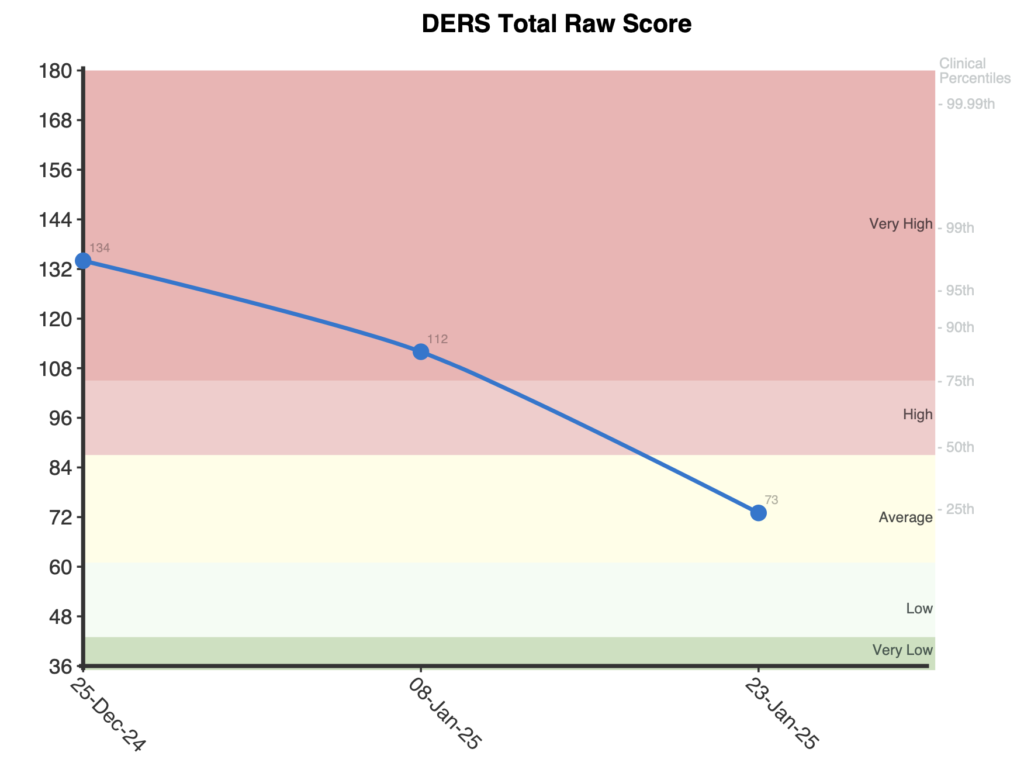
Total raw scores range from 36-180, with higher scores indicating greater difficulties in emotion regulation. Subscale raw scores have several ranges listed below:
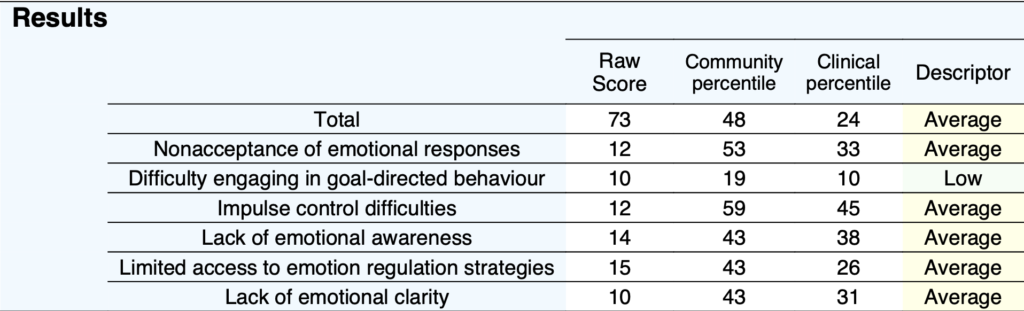
On first administration, a stacked bar graph shows the total and each of the six subscale scores in community percentiles. Percentiles give context to a client’s score, showing how they compare to their peers. For example, a percentile of 50 represents the typical level of difficulties with emotional regulation among adults in the community.
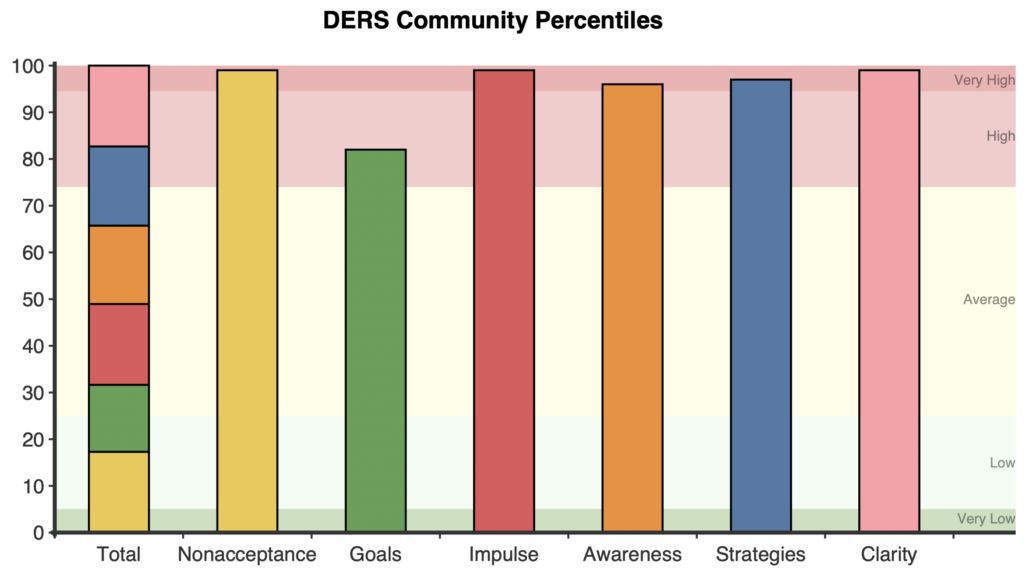
A horizontal comparison graph is also presented showing where a respondent’s score is in comparison to the normative and clinical samples.
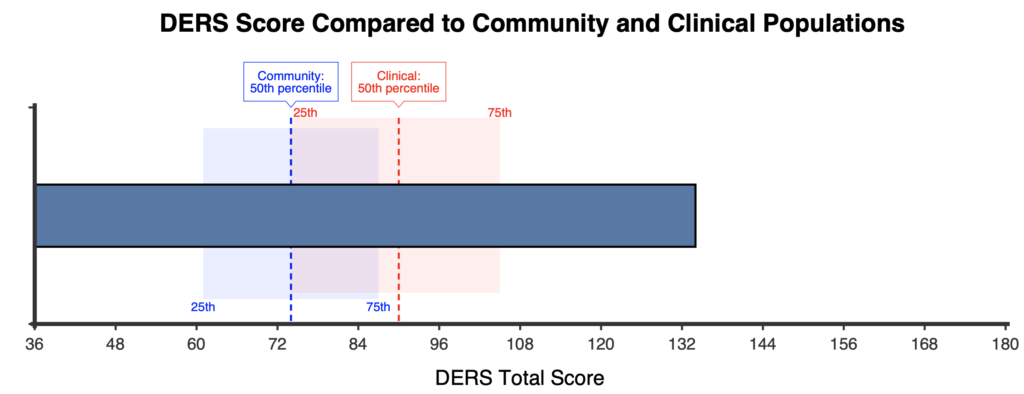
When administered more than once, a line graph is presented for the raw total score with clinical percentile labels on the right.
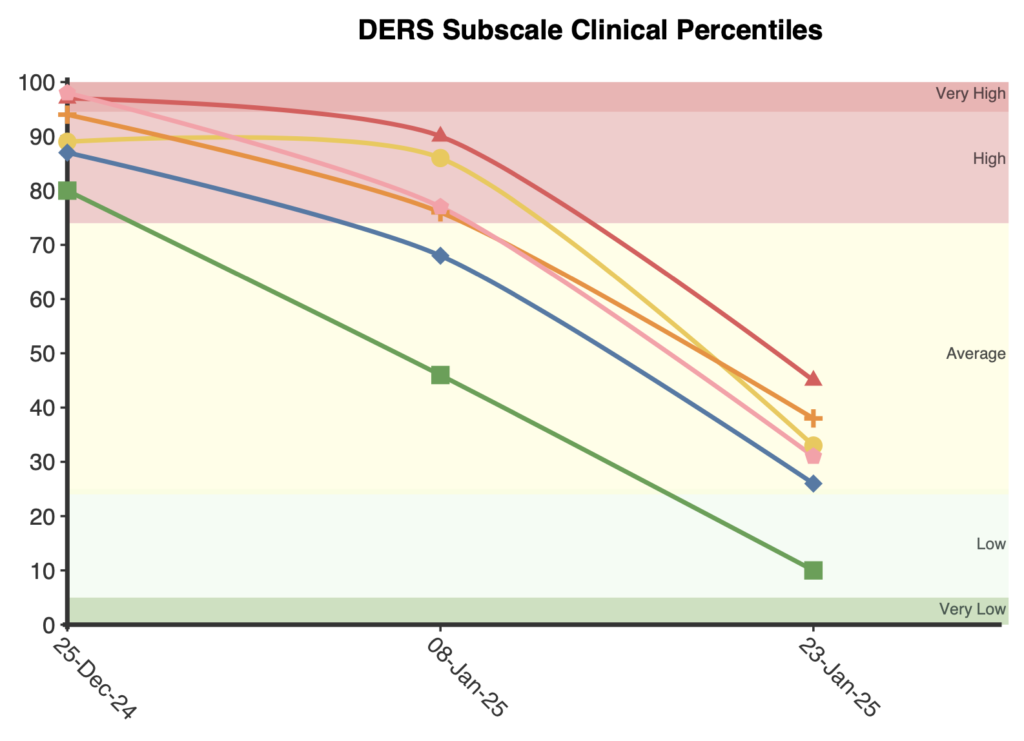
A second line graph is presented plotting each of the six subscales in clinical percentile terms.
Significant improvements or deterioration in the total score is indicated by shifts of half a standard deviation or greater (approximately 9 total score points or more) following the guidelines of the Minimally Important Difference (Turner et al., 2010).
Severity categories were created based on community percentiles derived from the combined community sample:
The DERS has strong psychometric properties across multiple studies in both clinical and non-clinical populations. Internal consistency for the full scale is consistently excellent, with Cronbach’s alpha values ranging from 0.93 to 0.95 (Fowler et al., 2014; Gratz & Roemer, 2004; Hallion et al., 2018). Subscale internal consistency ranges from generally good to excellent (alpha = 0.80-0.92).
Factor analytic studies have examined various structural models for the DERS. The original six-factor structure has shown acceptable fit across multiple populations (Fowler et al., 2014; Hallion et al., 2018; Neumann et al., 2010; Osborne et al., 2017). Other research has suggested that alternatives such as a five-factor structure and a bifactor model with one general emotion dysregulation factor and five specific factors (excluding Awareness) may also provide a good fit (Hallion et al., 2018; Osborne et al., 2017; Sörman et al., 2022). However, the original six-factor structure was shown to be acceptable in many studies (Fowler et al., 2014; Hallion et al., 2018; Neumann et al., 2010; Osborne et al., 2017) and remains widely used due to its comprehensive assessment.
Test-retest reliability over a period of 4-8 weeks is good for both the total score (r = 0.88) and subscale scores (r = 0.57-0.89; Gratz & Roemer, 2004). The scale shows good convergent validity with other measures of emotion regulation and related constructs. For example, scores correlate significantly with the Negative Mood Regulation Scale (r = -0.69) and measures of experiential avoidance (r = 0.60) (Gratz & Roemer, 2004).
Clinical norms have been reported from a sample of treatment-seeking adults by Hallion et al. (2018). The authors reported a mean total score of 89.33 (SD = 22.64). Table 1 provides further details, including subscale scores from this sample.
Community norms were established by Gratz and Roemer (2004) in their original validation using 375 undergraduate students in the United States (total score M=78.71(20.22). More recent large-scale studies have also reported community norms, such as 1,049 undergraduate students (total score M=75.26(17.15) from Australia in Burton et al. (2022) and 843 community adults (total score M=70.22(20.24) from the United States in Sörman et al. (2022).
For the total score, NovoPsych calculated a weighted mean and pooled standard deviation to combine community sample data from Gratz & Roemer (2004), Sörman et al (2022) and Burton et al (2022). Total score severity categories were created based on the percentile ranges of this combined sample (M=73.80(18.89)).
For subscales, data is reported for both clinical (Hallion et al 2018) and community (Gratz & Roemer, 2004) samples, and are detailed in table 1 of the technical review.
Gratz, K. L., & Roemer, L. (2004). Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment, 26(1), 41-54.
Bardeen, J. R., Fergus, T. A., & Orcutt, H. K. (2012). An examination of the latent structure of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment, 34(3), 382-392. https://doi.org/10.1007/s10862-012-9280-y
Bartholomew, E., Hegarty, D., Buchanan, B., Baker, S., Smyth, C. (2025). A Review of the Difficulties in Emotion Regulation Scale (DERS): Percentile-Based Severity Ranges, Clinical and Community Normative Data and Qualitative Descriptors.
Burton, A. L., Brown, R., & Abbott, M. J. (2022). Overcoming difficulties in measuring emotional regulation: Assessing and comparing the psychometric properties of the DERS long and short forms. Cogent Psychology, 9(1), 2060629. https://doi.org/10.1080/23311908.2022.2060629
Fowler, J. C., Charak, R., Elhai, J. D., Allen, J. G., Frueh, B. C., & Oldham, J. M. (2014). Construct validity and factor structure of the difficulties in emotion regulation scale among adults with severe mental illness. Journal of Psychiatric Research, 58, 175-180. https://doi.org/10.1016/j.jpsychires.2014.07.029
Gratz, K. L., & Roemer, L. (2004). Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment, 26(1), 41-54. https://doi.org/10.1023/B:JOBA.0000007455.08539.94
Hallion, L. S., Steinman, S. A., Tolin, D. F., & Diefenbach, G. J. (2018). Psychometric properties of the difficulties in emotion regulation scale (DERS) and its short forms in adults with emotional disorders. Frontiers in Psychology, 9, 539. https://doi.org/10.3389/fpsyg.2018.00539
Neumann, A., van Lier, P. A., Gratz, K. L., & Koot, H. M. (2010). Multidimensional assessment of emotion regulation difficulties in adolescents using the difficulties in emotion regulation scale. Assessment, 17(1), 138-149. https://doi.org/10.1177/1073191109349579
Osborne, T. L., Michonski, J., Sayrs, J., Welch, S. S., & Anderson, L. K. (2017). Factor structure of the difficulties in emotion regulation scale (DERS) in adult outpatients receiving dialectical behavior therapy (DBT). Journal of Psychopathology and Behavioral Assessment, 39(4), 355-371. https://doi.org/10.1007/s10862-017-9586-x
Perez, J., Venta, A., Garnaat, S., & Sharp, C. (2012). The difficulties in emotion regulation scale: Factor structure and association with nonsuicidal self-injury in adolescent inpatients. Journal of Psychopathology and Behavioral Assessment, 34(3), 393-404. https://doi.org/10.1007/s10862-012-9292-7
Skutch, J. M., Wang, S. B., Buqo, T., Haynos, A. F., & Papa, A. (2019). Which brief is best? Clarifying the use of three brief versions of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment, 41(3), 485-494. https://doi.org/10.1007/s10862-019-09736-z
Sörman, K., Garke, M. Å., Isacsson, N. H., Jangard, S., Bjureberg, J., Hellner, C., Sinha, R., & Jayaram-Lindström, N. (2022). Measures of emotion regulation: Convergence and psychometric properties of the difficulties in emotion regulation scale and emotion regulation questionnaire. Journal of Clinical Psychology, 78(2), 201-217. https://doi.org/10.1002/jclp.23206
NovoPsych’s mission is to help mental health services use psychometric science to improve client outcomes.
© 2023 Copyright – NovoPsych – All rights reserved